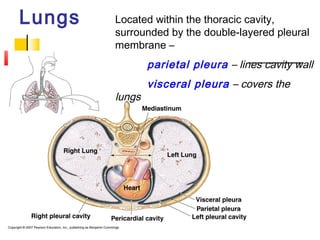
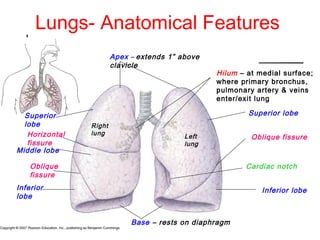
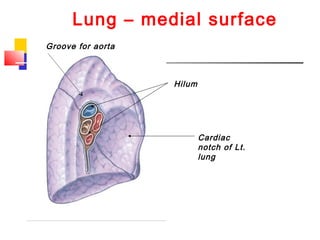
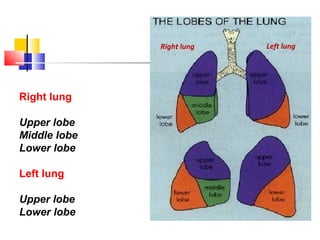
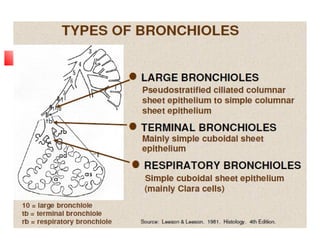
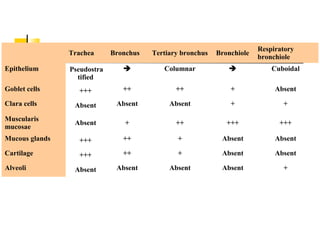
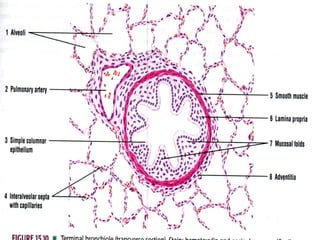
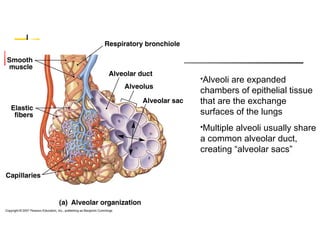
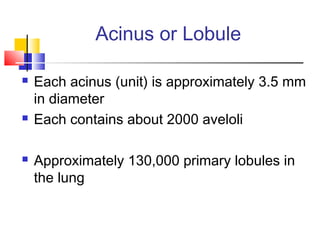
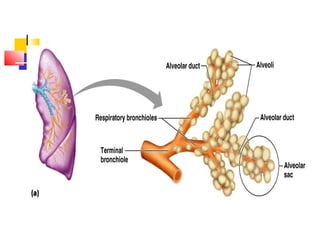
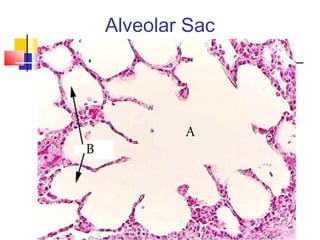
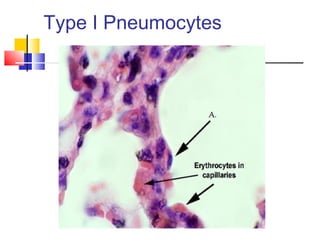
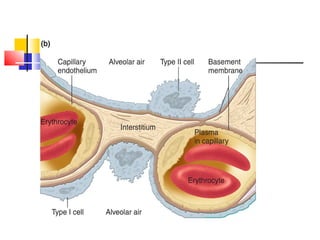
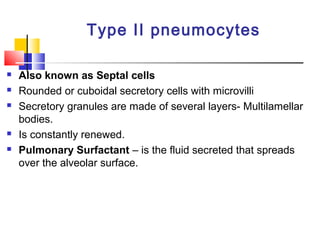
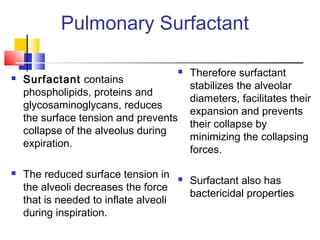
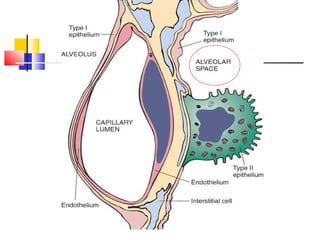
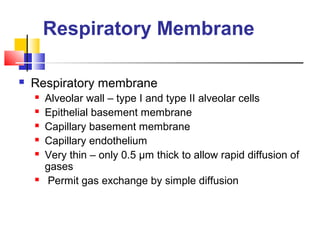
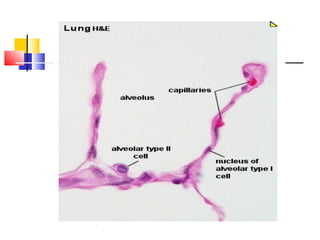
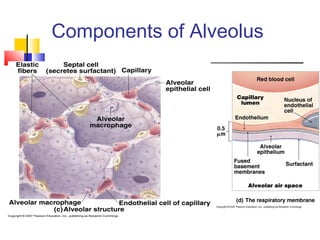
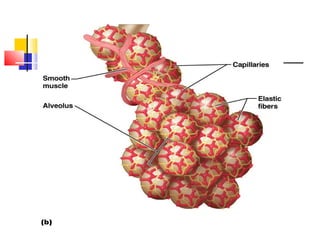
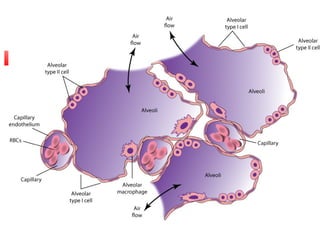
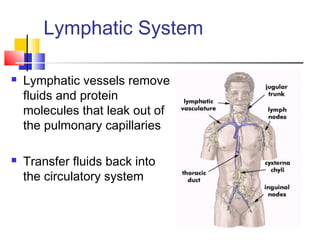
The lungs are located in the thoracic cavity and surrounded by the pleural membranes. They have an apex, base, lobes, and hilum where structures enter and exit. The lungs contain branching airways down to terminal bronchioles and alveoli, which are the gas exchange surfaces. Alveoli are made of type I and II cells and contain surfactant. The blood-air barrier is very thin to allow for gas exchange by diffusion. The lungs receive blood flow from the pulmonary and bronchial circulations and have lymphatic drainage.