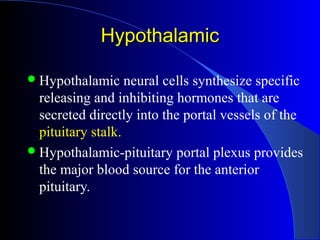
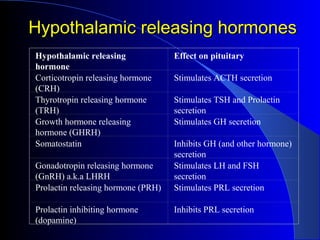
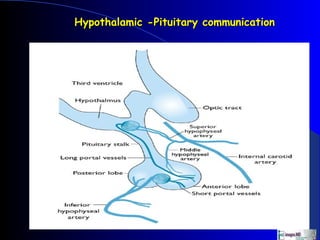
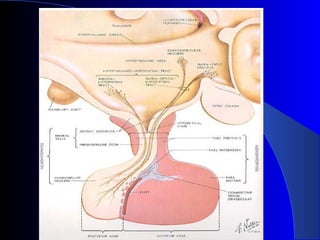
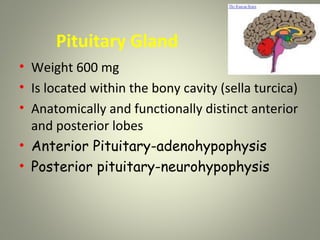
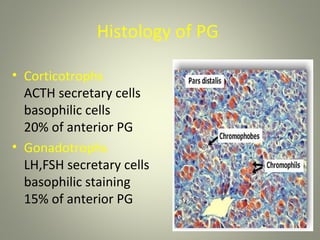
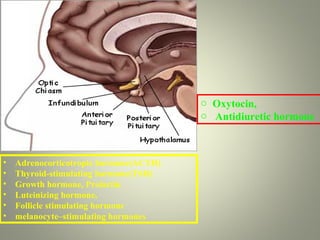
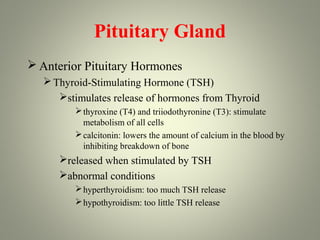
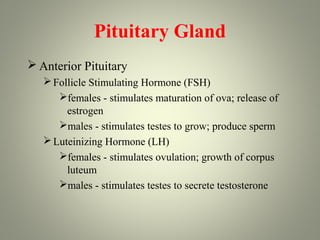
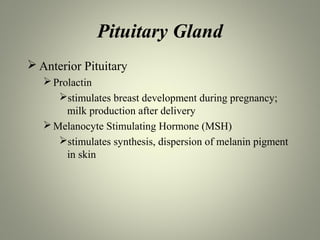
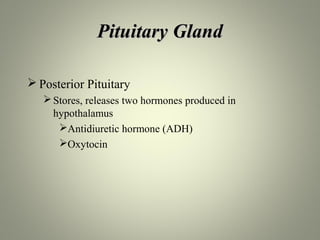
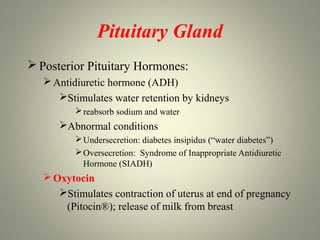
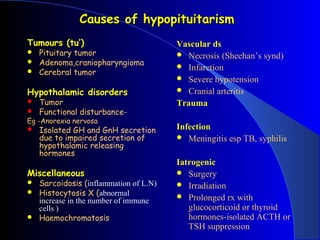
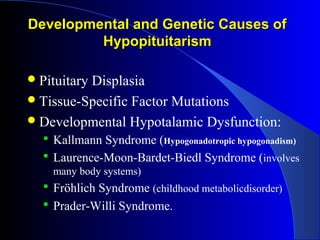
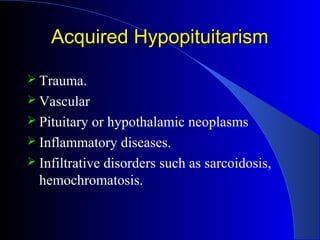
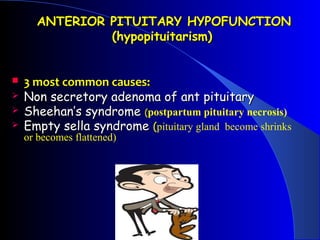
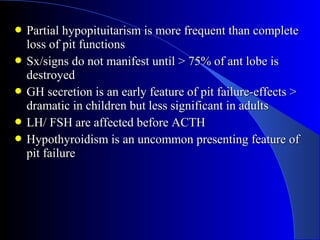
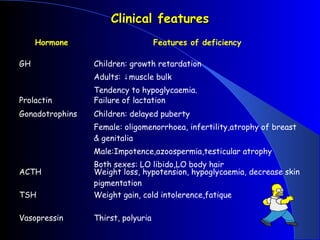
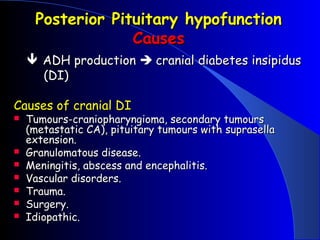
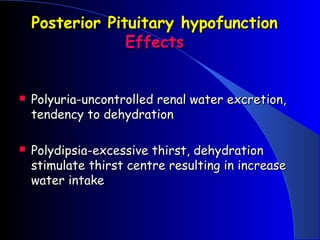
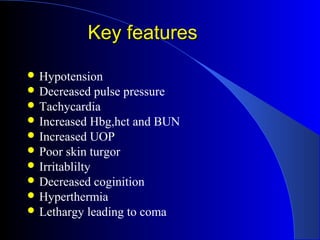
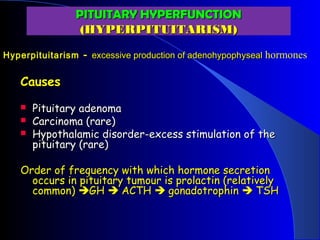
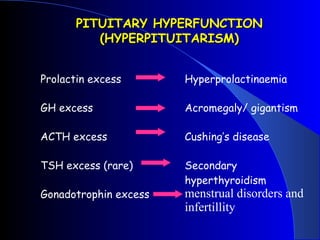
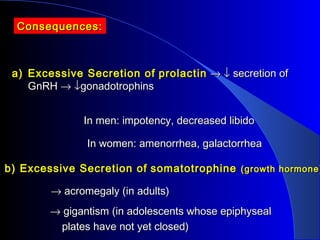
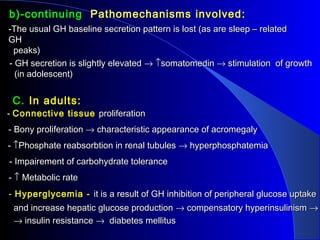
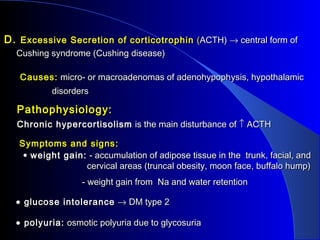
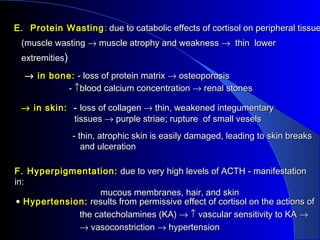
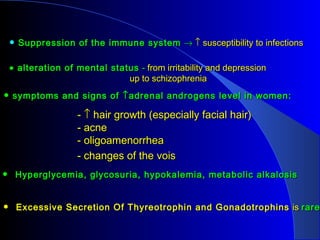
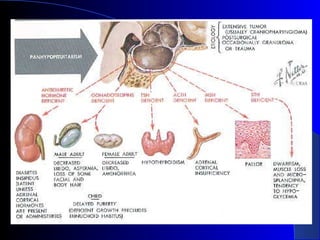
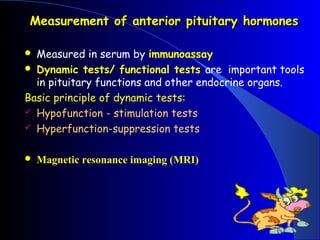
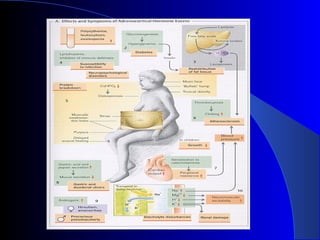
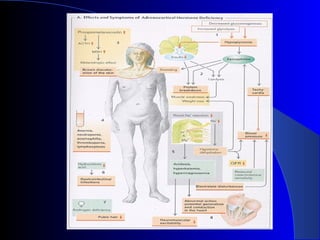
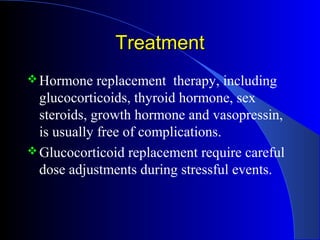
The document discusses the pituitary gland and pituitary diseases. It begins by providing an overview of the pituitary gland, noting that it is located at the base of the brain and controls other endocrine glands by releasing hormones into the bloodstream. It then discusses specific pituitary diseases including anterior and posterior pituitary hypofunction, as well as pituitary hyperfunction. Anterior pituitary hypofunction can be caused by tumors, vascular issues, or trauma/infection and results in hormone deficiencies. Posterior pituitary hypofunction impacts antidiuretic hormone and causes diabetes insipidus. Pituitary hyperfunction includes excess secretion of hormones like prolactin, growth hormone, ACTH, and TSH, leading to conditions such as acromegaly, Cushing