This document discusses several types of autoimmune encephalitis:
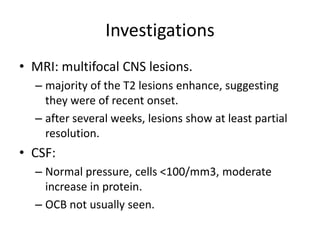
- Acute disseminated encephalomyelitis (ADEM) typically occurs after infections or vaccinations and is characterized by inflammation and demyelination in the central nervous system.
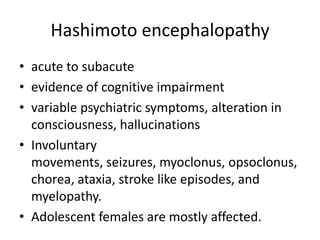
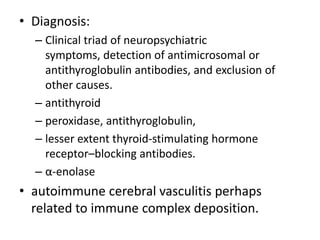
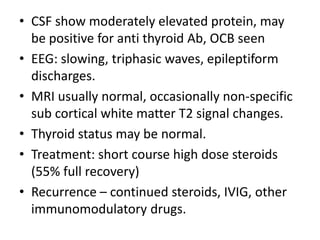
- Hashimoto's encephalopathy presents with cognitive and psychiatric symptoms and is associated with anti-thyroid antibodies.
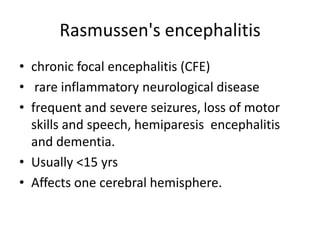
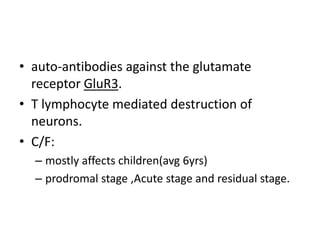
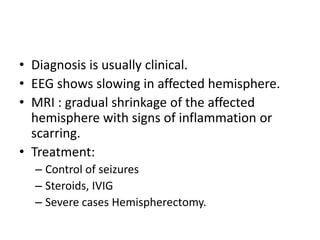
- Rasmussen's encephalitis is a rare disease that causes seizures, neurological deficits, and brain inflammation localized to one hemisphere, typically in children.
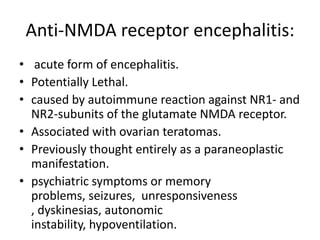
- Anti-NMDA receptor encephalitis is an acute form associated with ovarian teratomas that presents with psychiatric symptoms, seizures, and dyskinesias.
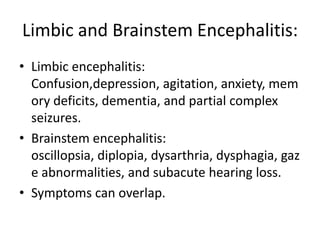
![• MRI:
– unilateral or bilateral mesial temporal lobe
abnormalities on T2-weighted and FLAIR images’
– The temporal-limbic regions may be hypointense on
T1-weighted sequences and may enhance with
contrast.
• Associated with testicular germ cell
tumors, Hodgkin lymphoma, thymoma.
• Antigens:
– Intra cellular: Hu, Ma2, CV2/CRMP5
– Cell surface antigens: AMPA receptors, leucine-rich
glioma inactivated 1 (LGI1) and γ-aminobutyric acid
type B [GABA-B] receptors.](https://image.slidesharecdn.com/autoimmuneencephalitides-130623114238-phpapp01/85/Autoimmune-encephalitides-18-320.jpg)