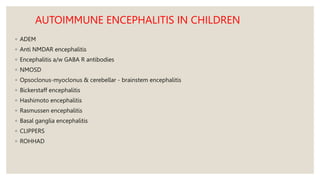
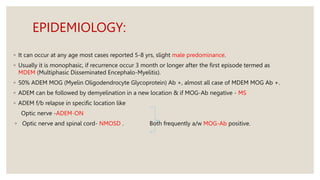
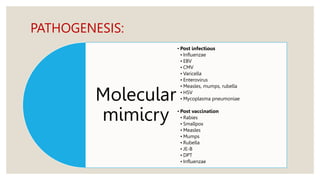
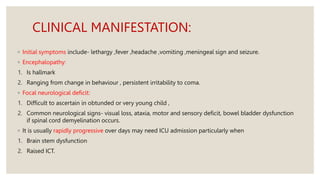
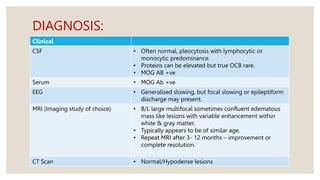
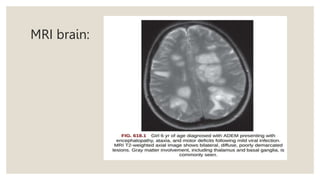
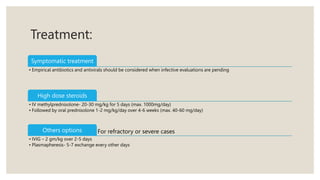
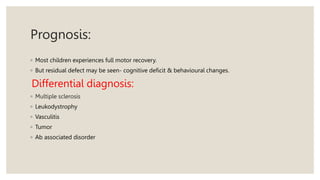
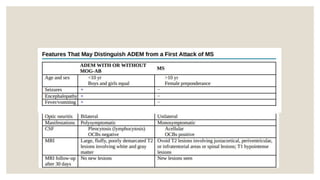
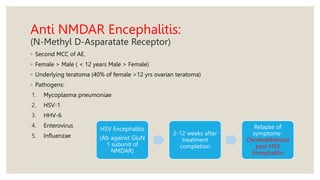
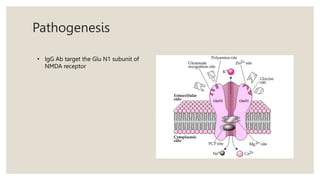
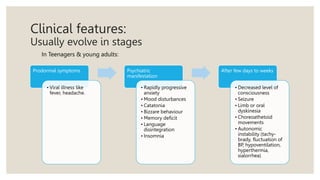
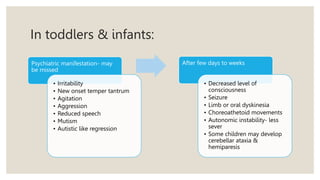
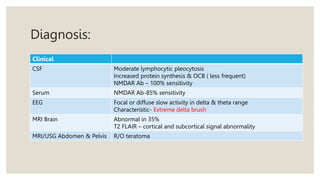
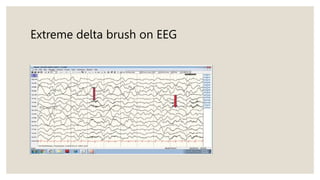
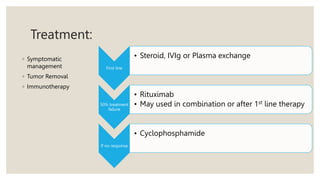
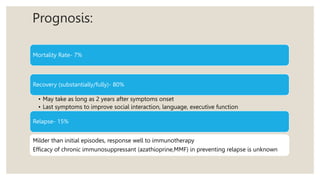
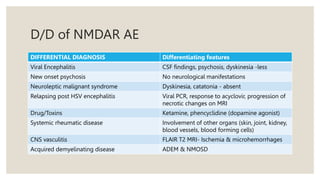
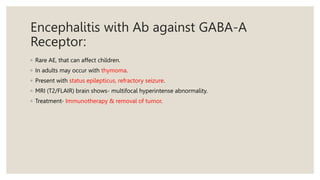
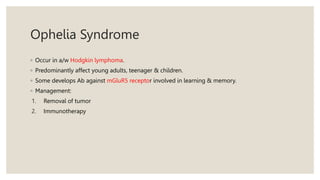
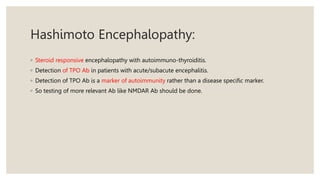
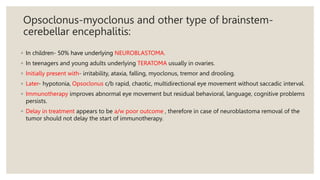
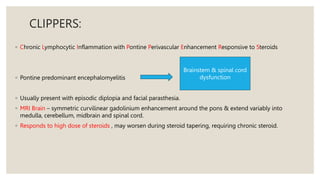
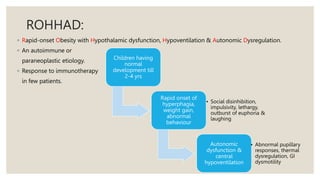
Autoimmune encephalitis is a neurological syndrome in children characterized by autoimmune responses against neuronal components, leading to various clinical manifestations and potentially severe outcomes. The document details types of autoimmune encephalitis, epidemiology, pathogenesis, clinical presentations, diagnostic methods, treatments, and prognosis, highlighting several specific entities such as ADEM and anti-NMDAR encephalitis. It underscores the importance of prompt diagnosis and treatment to improve recovery outcomes, particularly in the pediatric population.