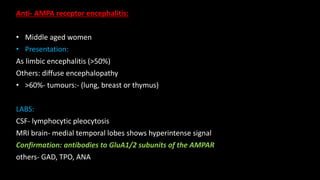
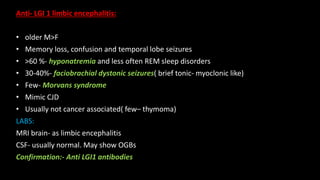
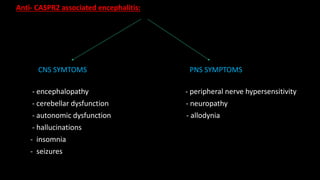
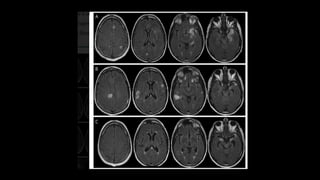
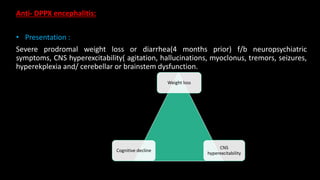
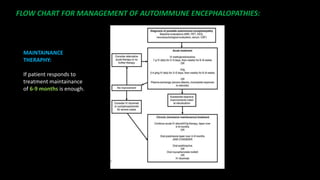
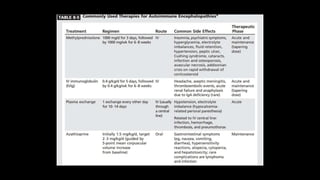
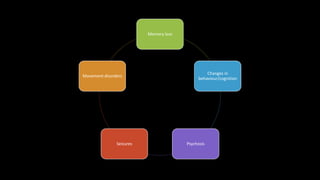
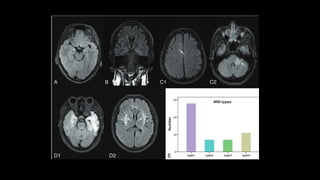
The document discusses autoimmune encephalitis, a group of neuro-psychiatric disorders characterized by symptoms such as memory loss, seizures, and changes in behavior, with reversibility achievable through immunotherapy. Various types of autoimmune encephalitis are detailed, including anti-NMDAR and anti-GABAB receptor encephalitis, highlighting their common presentations, laboratory findings, and treatment strategies. Emphasis is placed on the importance of early diagnosis and treatment to improve patient outcomes.
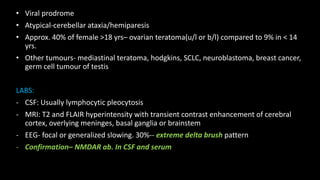

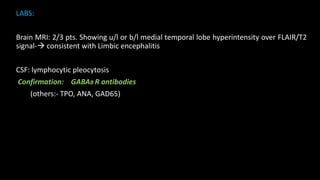
![Anti GABAB receptor encephalitis:
• Usually >60 yrs and M:F
• > 50 %- tumours
• Presentation
Memory loss
Confusion Typical of LIMBIC ENCEPHALITIS
Seizures[TLE]
Rarely: ataxia or opsoclonus-myoclonus syn.](https://image.slidesharecdn.com/autoimmuneencephalitis-220906174746-9505a2a3/85/AUTOIMMUNE-ENCEPHALITIS-9-320.jpg)