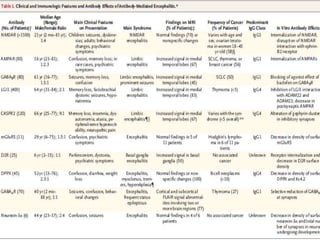
- Antibody-mediated encephalitides are inflammatory brain diseases characterized by neuropsychiatric symptoms associated with antibodies against neuronal proteins. The estimated annual incidence is 5-8 cases per 100,000 people.
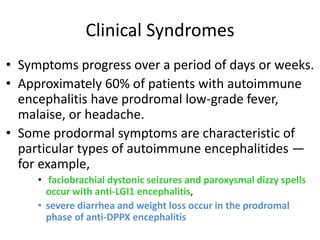
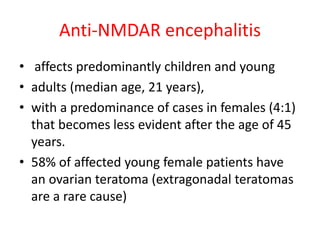
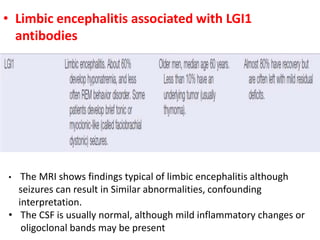
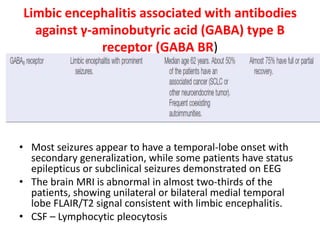
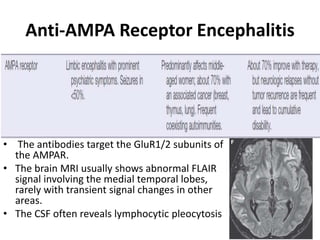
- Common forms include anti-NMDAR encephalitis, which predominantly affects young females and can cause psychiatric symptoms, seizures, and decreased consciousness. Limbic encephalitis usually affects older patients and causes confusion, behavioral changes, and memory impairment.
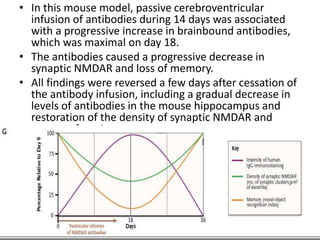
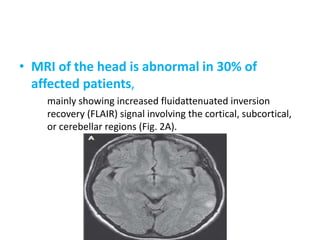
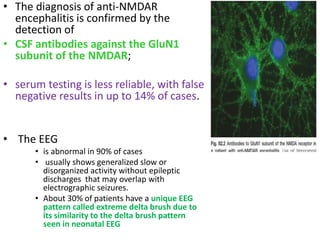
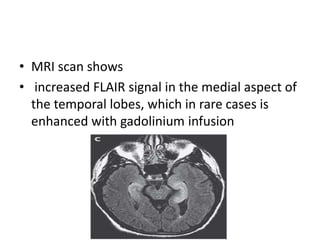
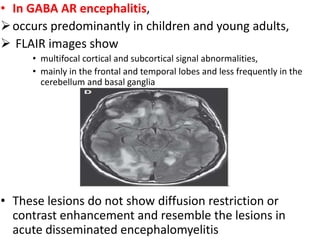
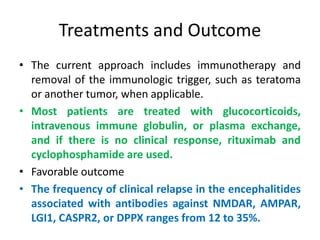
- Diagnosis involves detecting antibodies in CSF or serum and MRI/EEG findings. Treatment includes immunotherapy, tumor removal if applicable, and medications like steroids, IVIg, or rituximab. Outcomes can be favorable