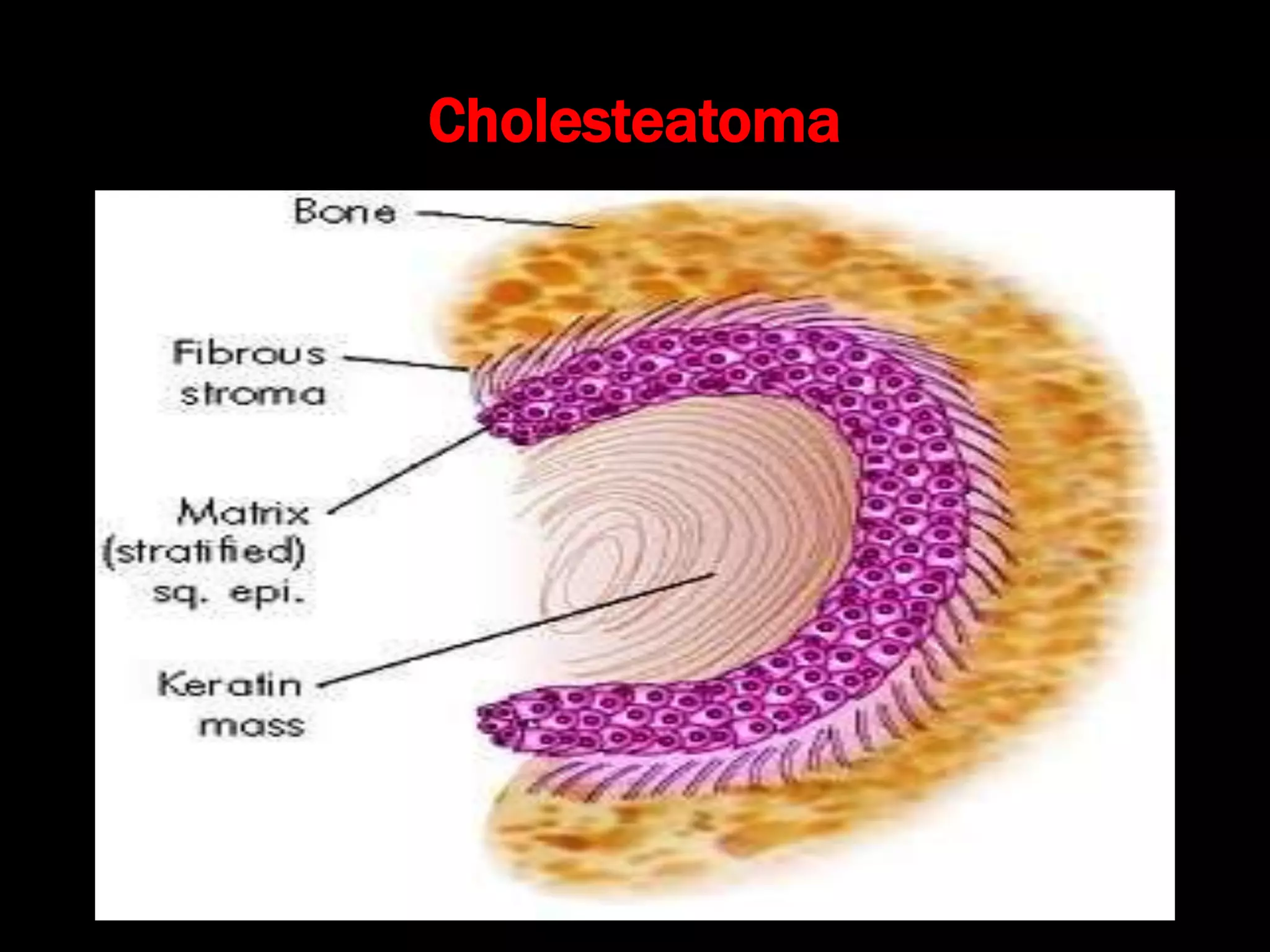
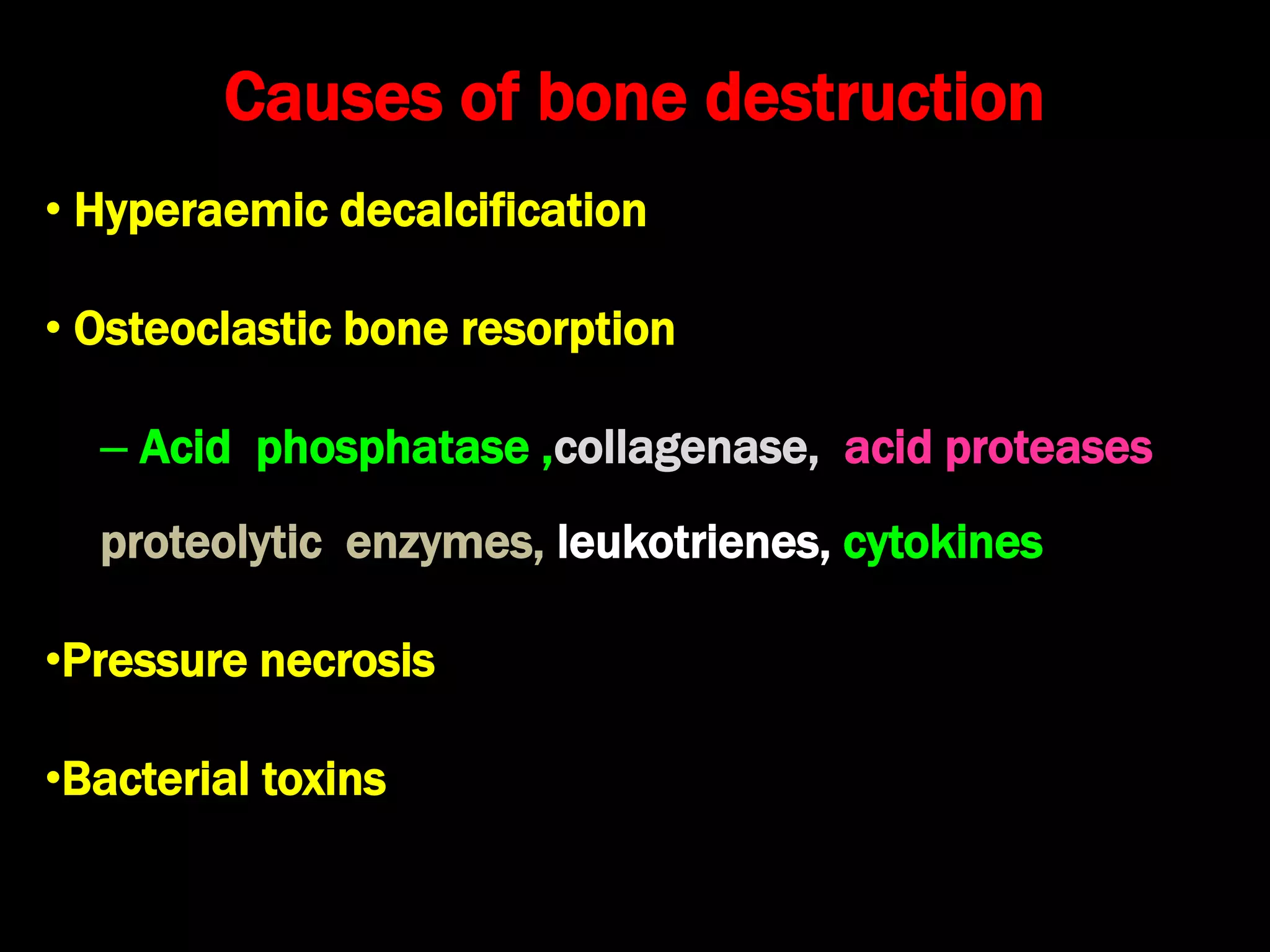
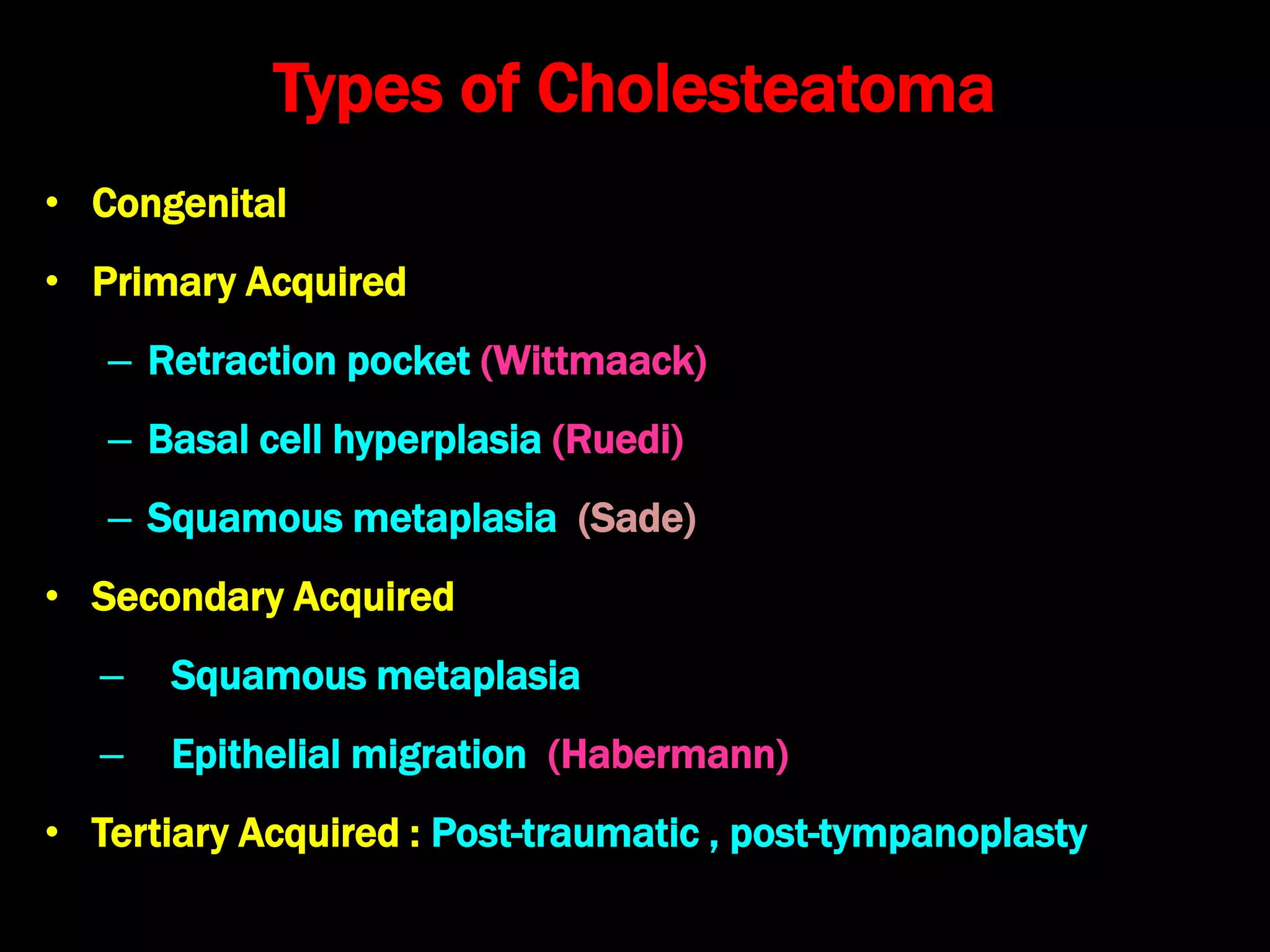
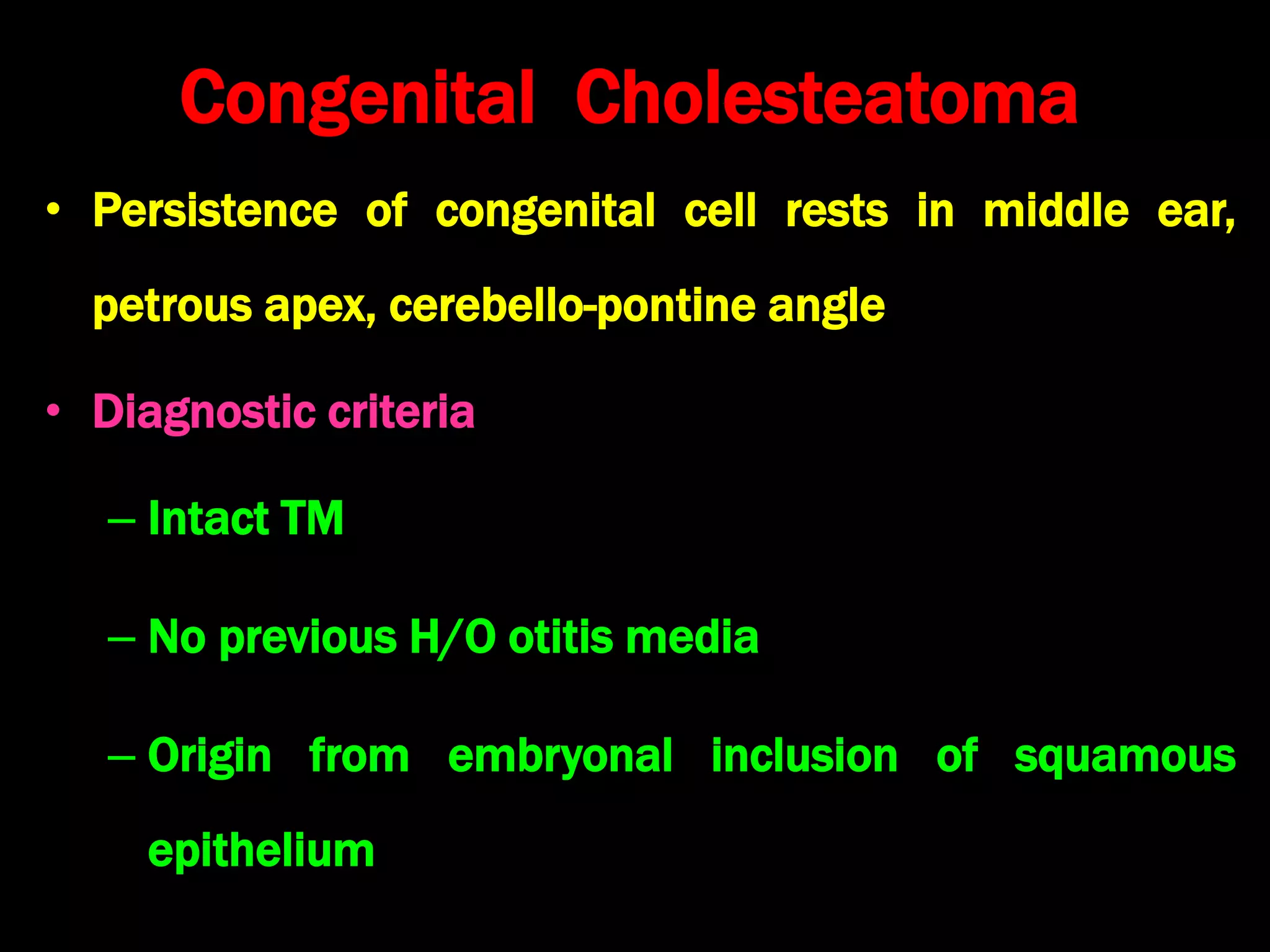
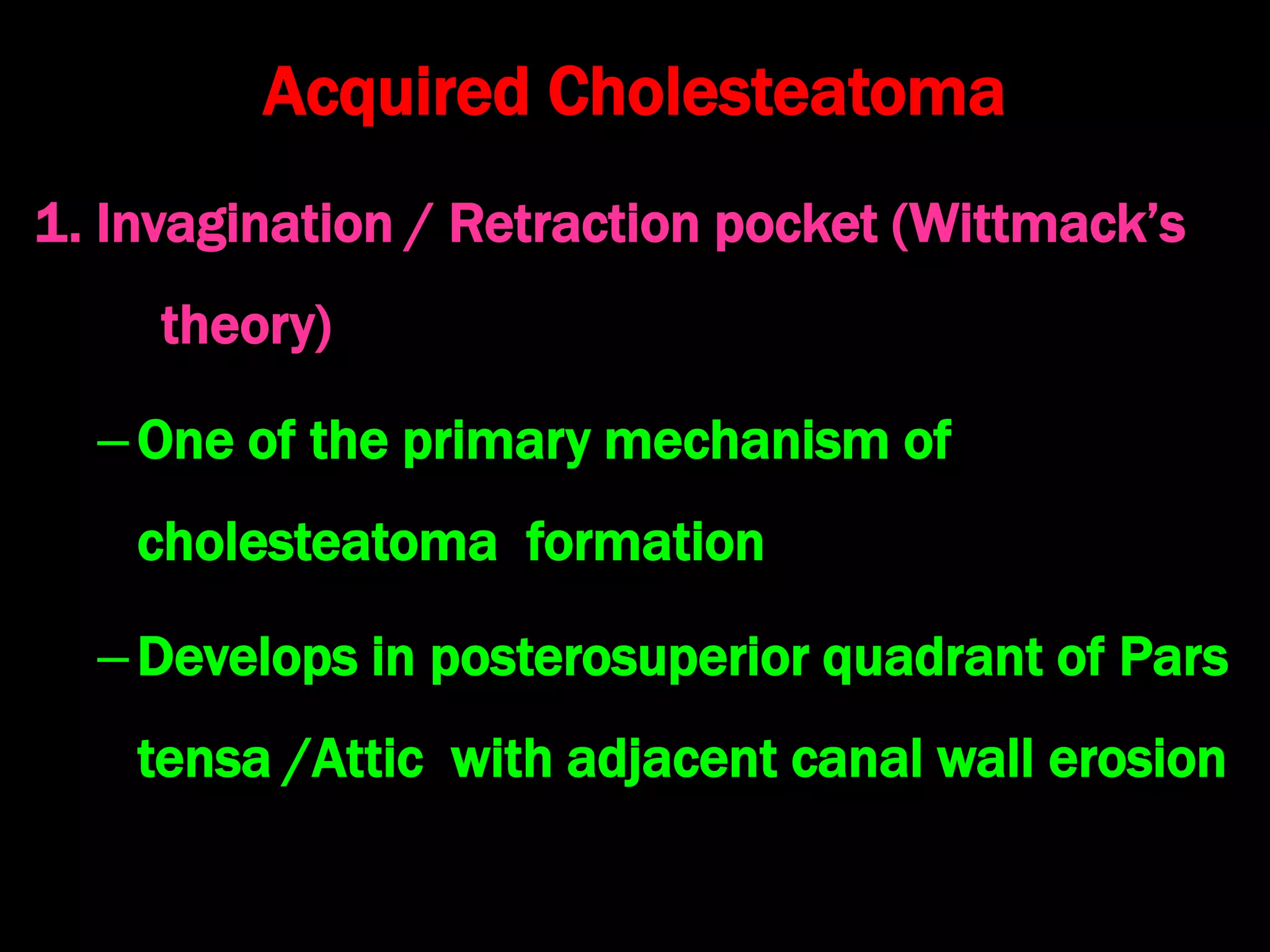
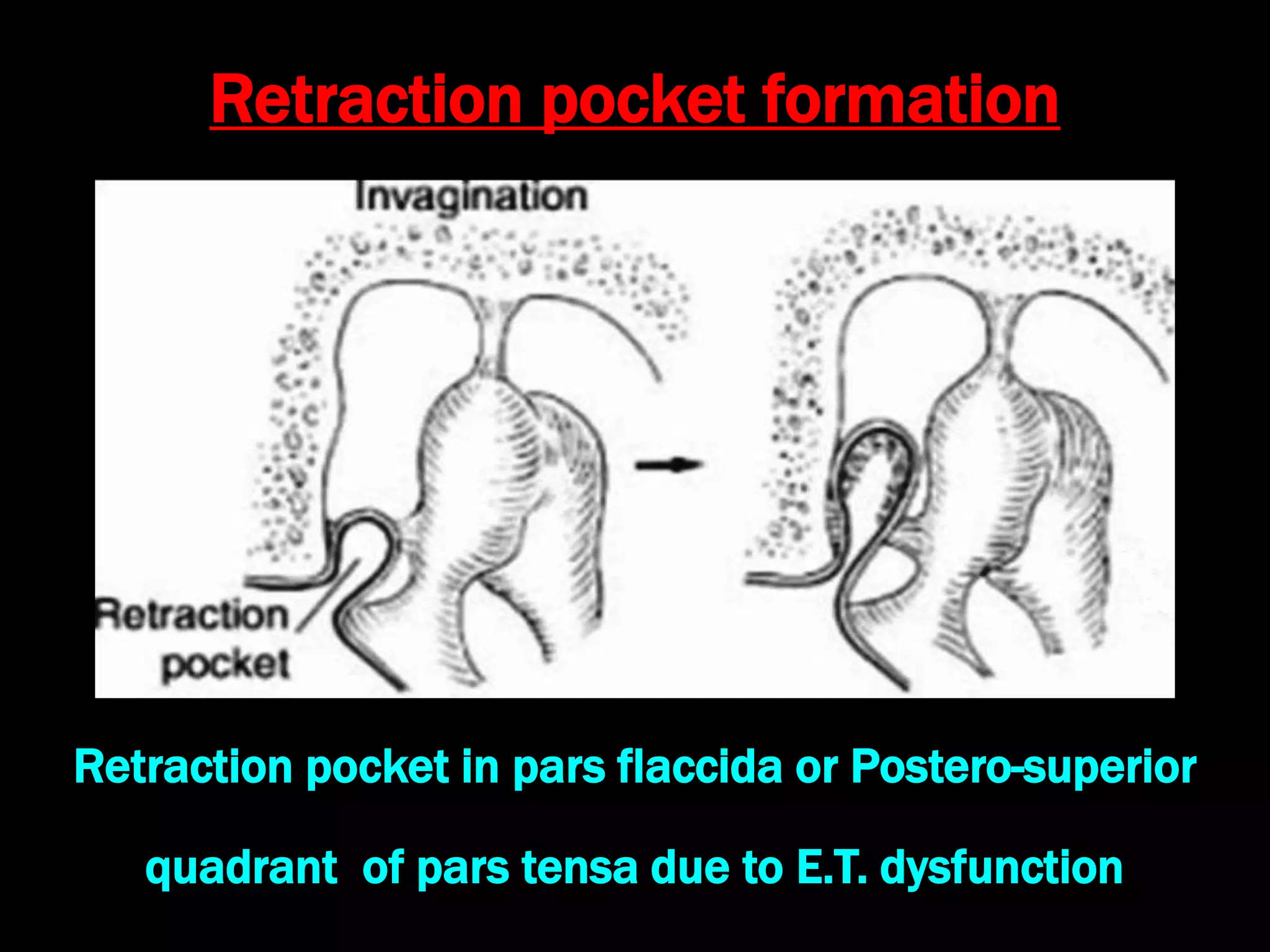
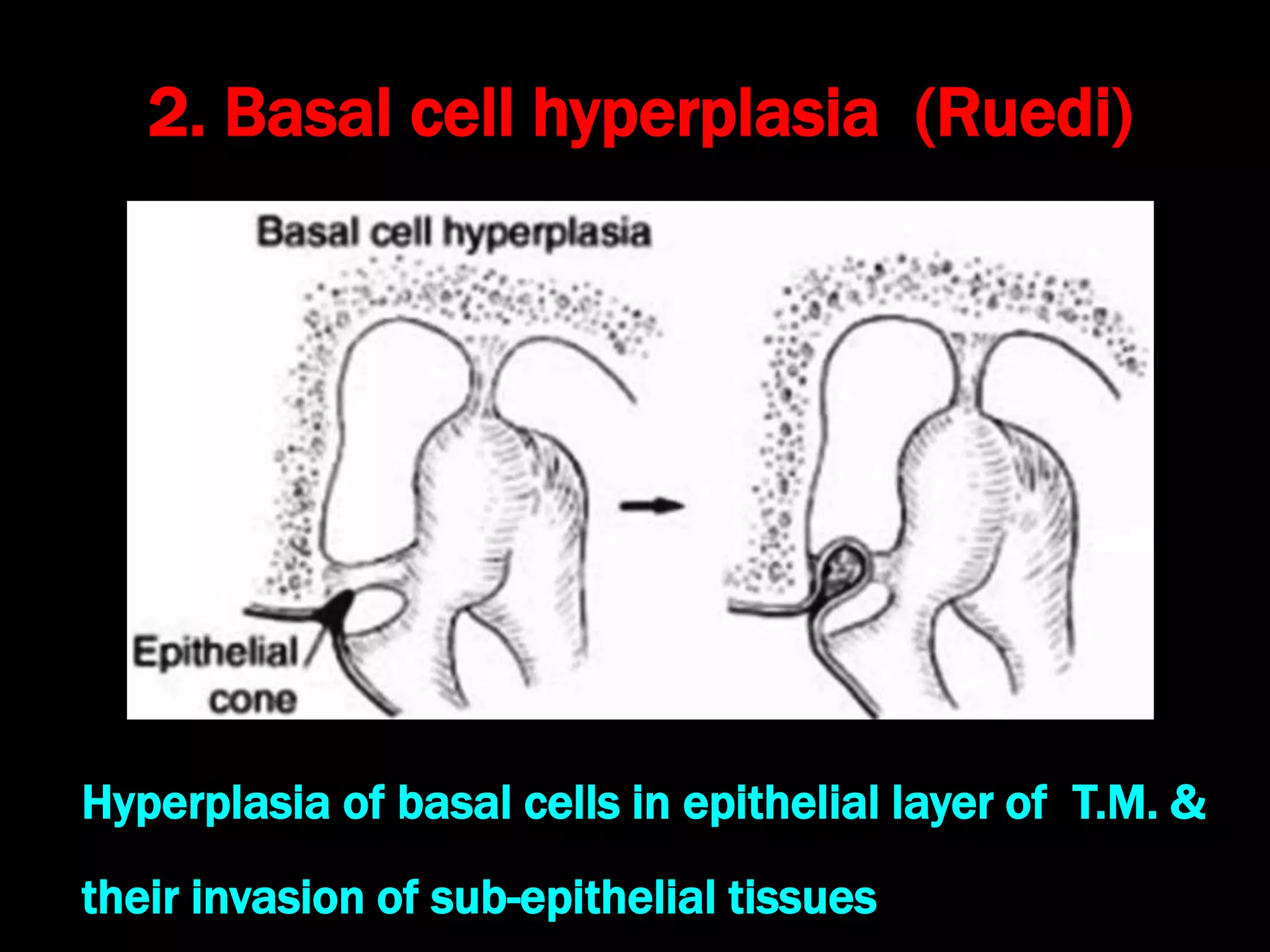
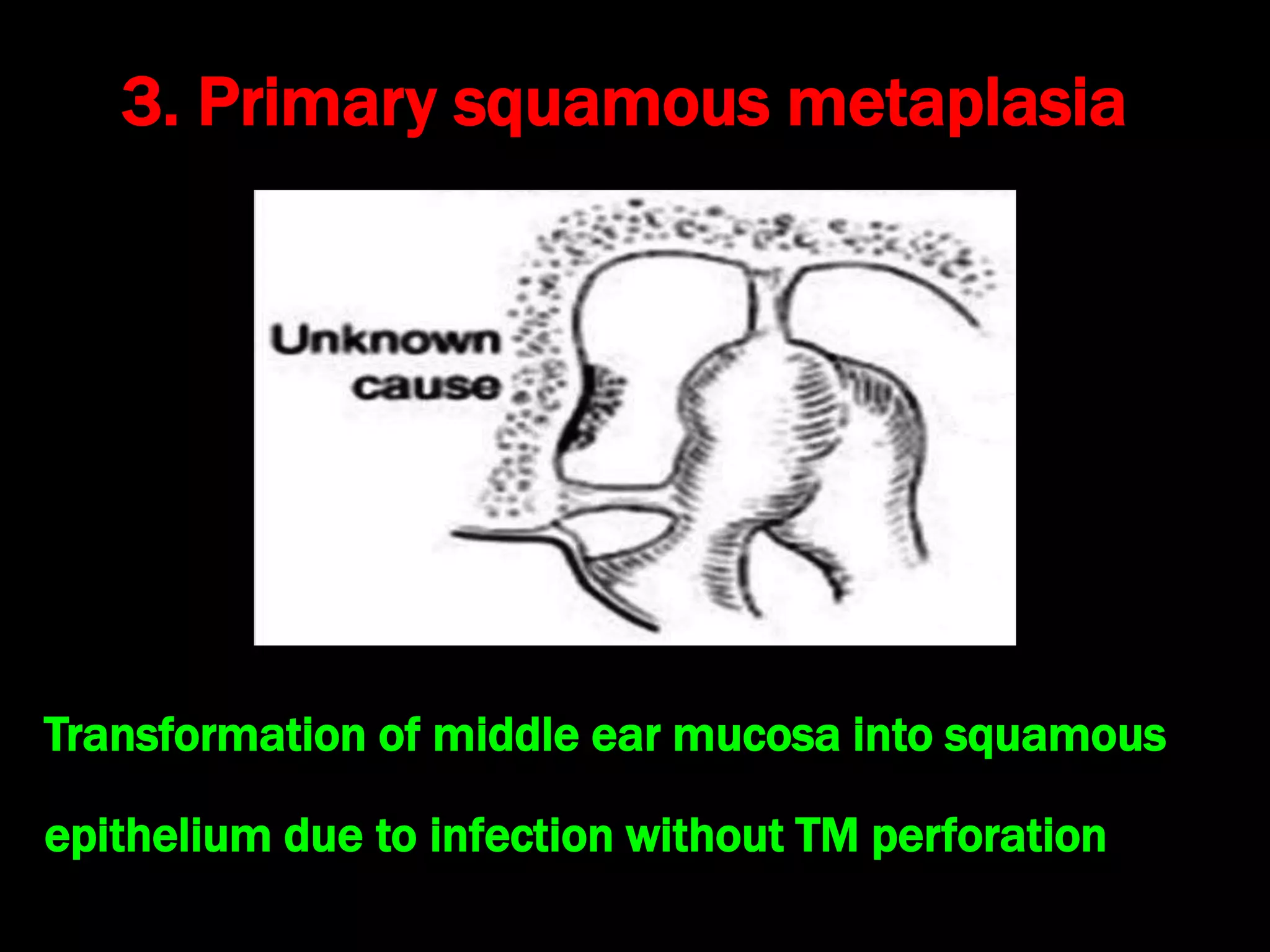
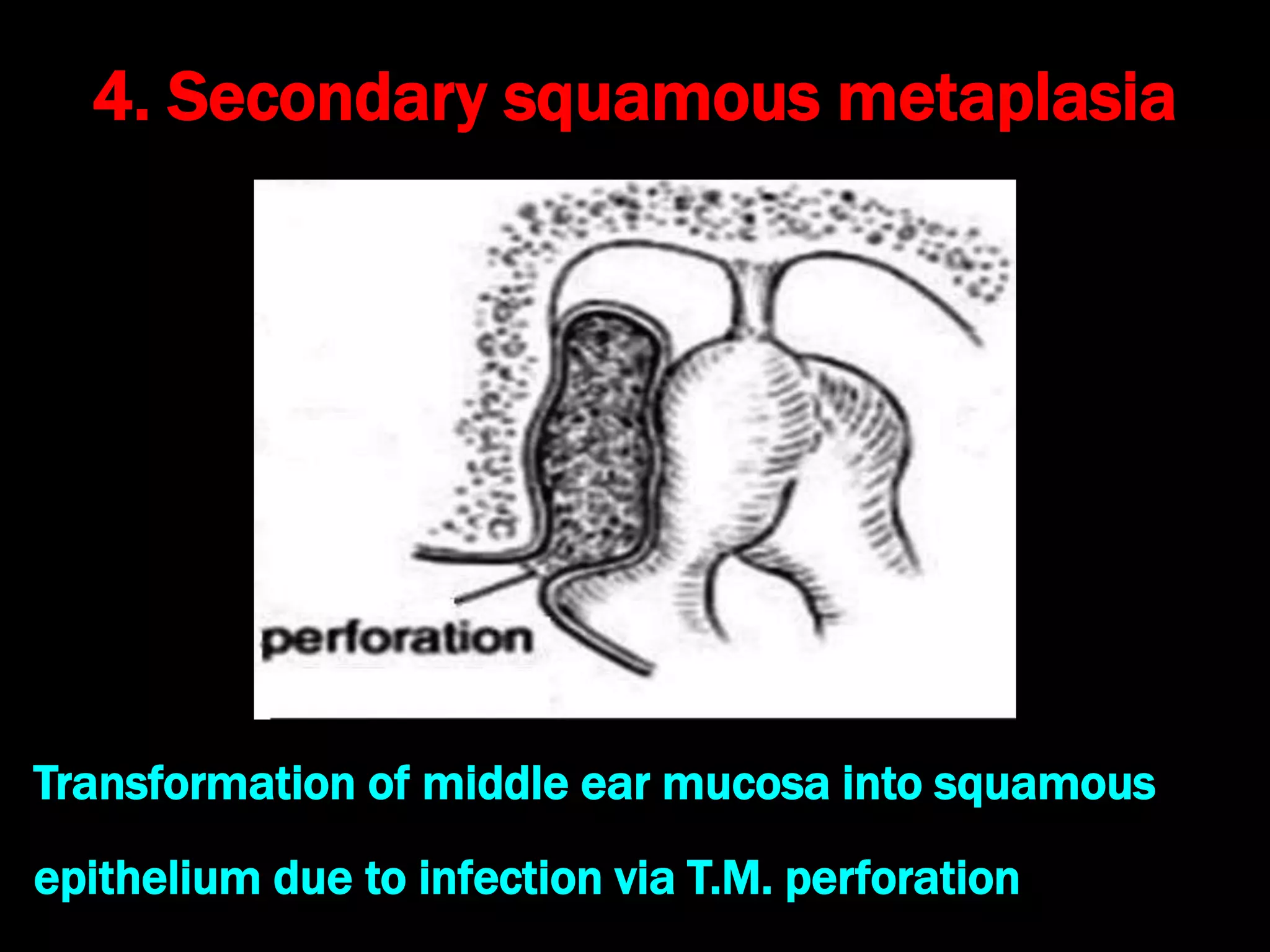
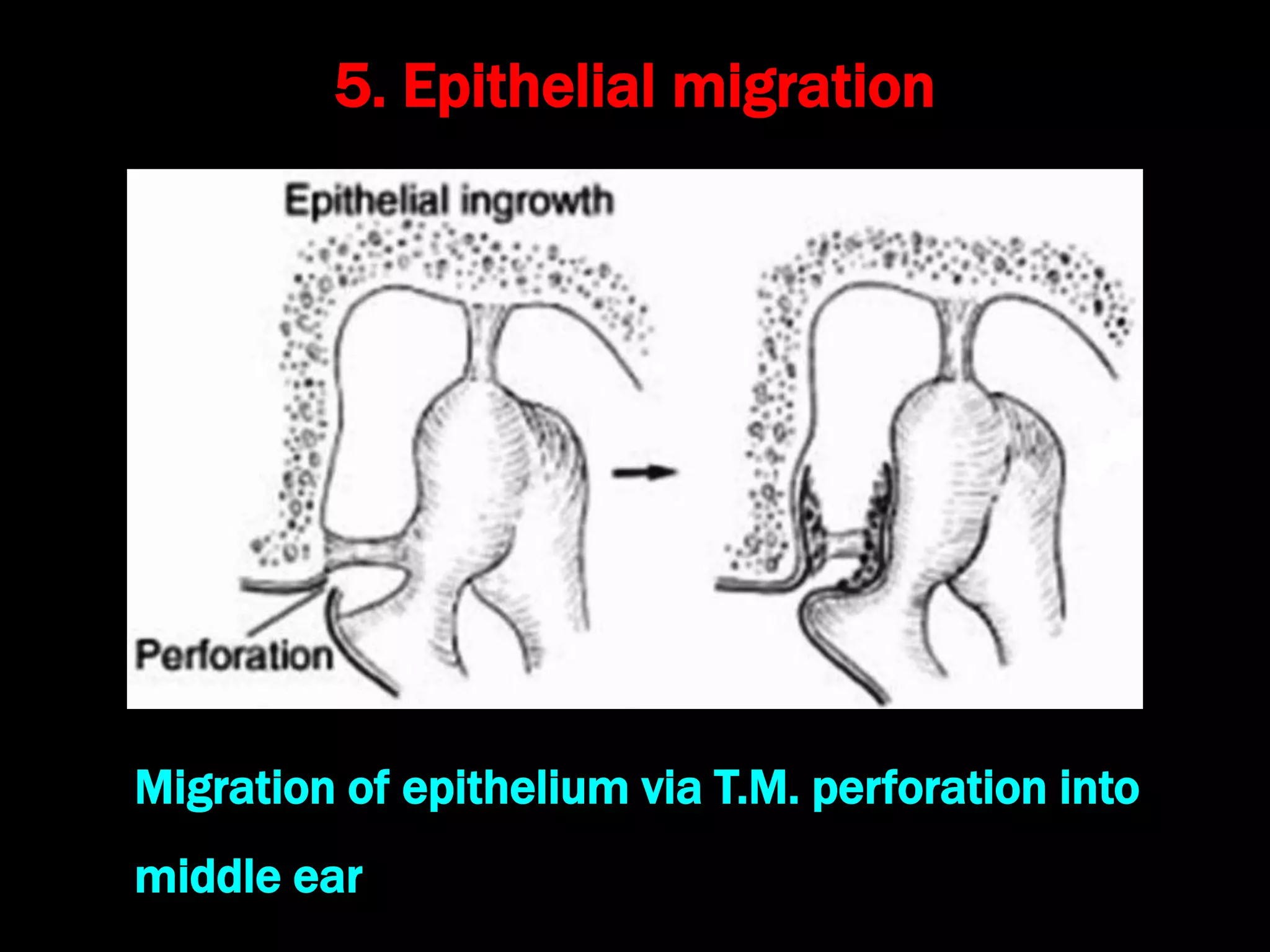
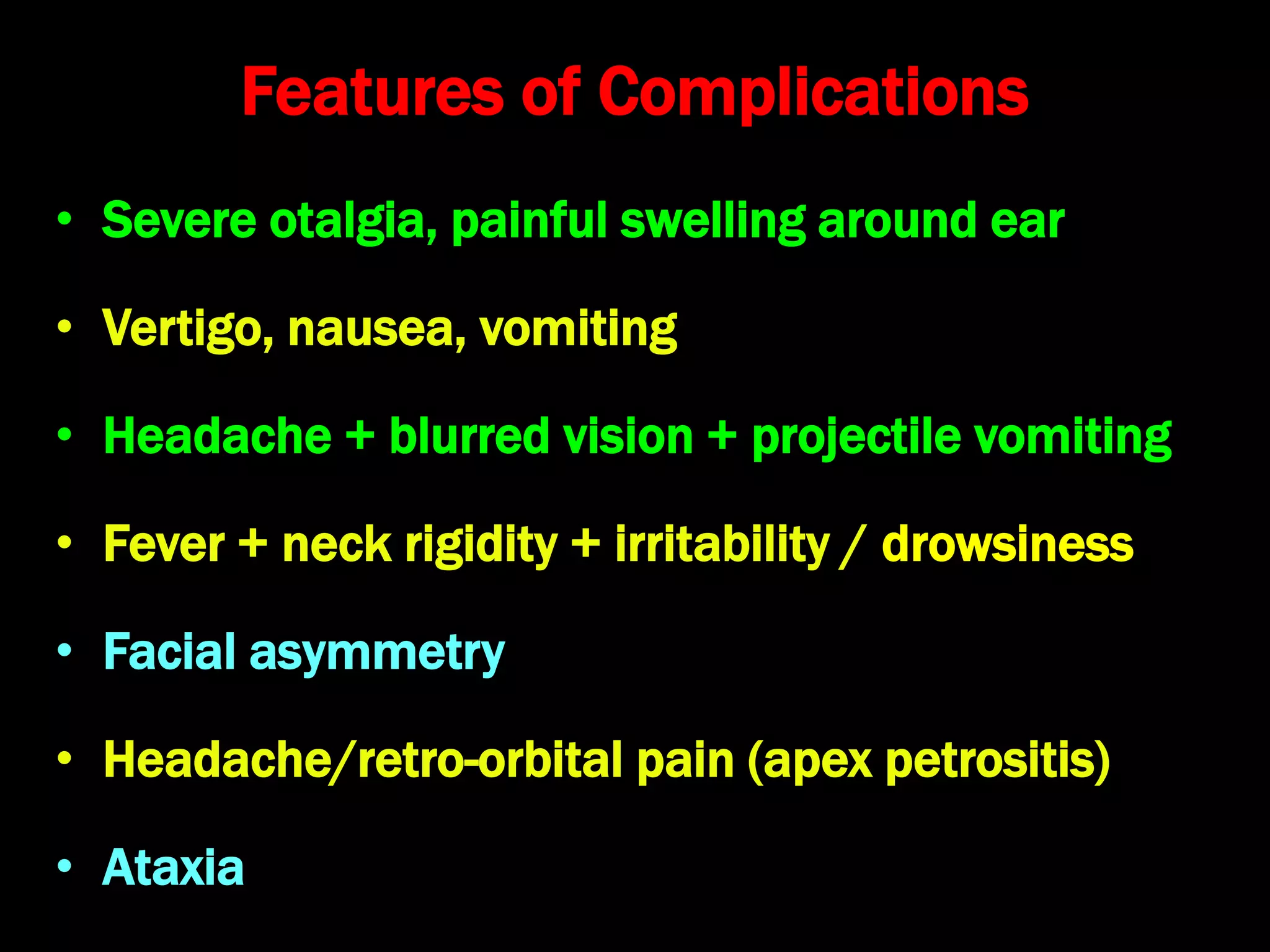
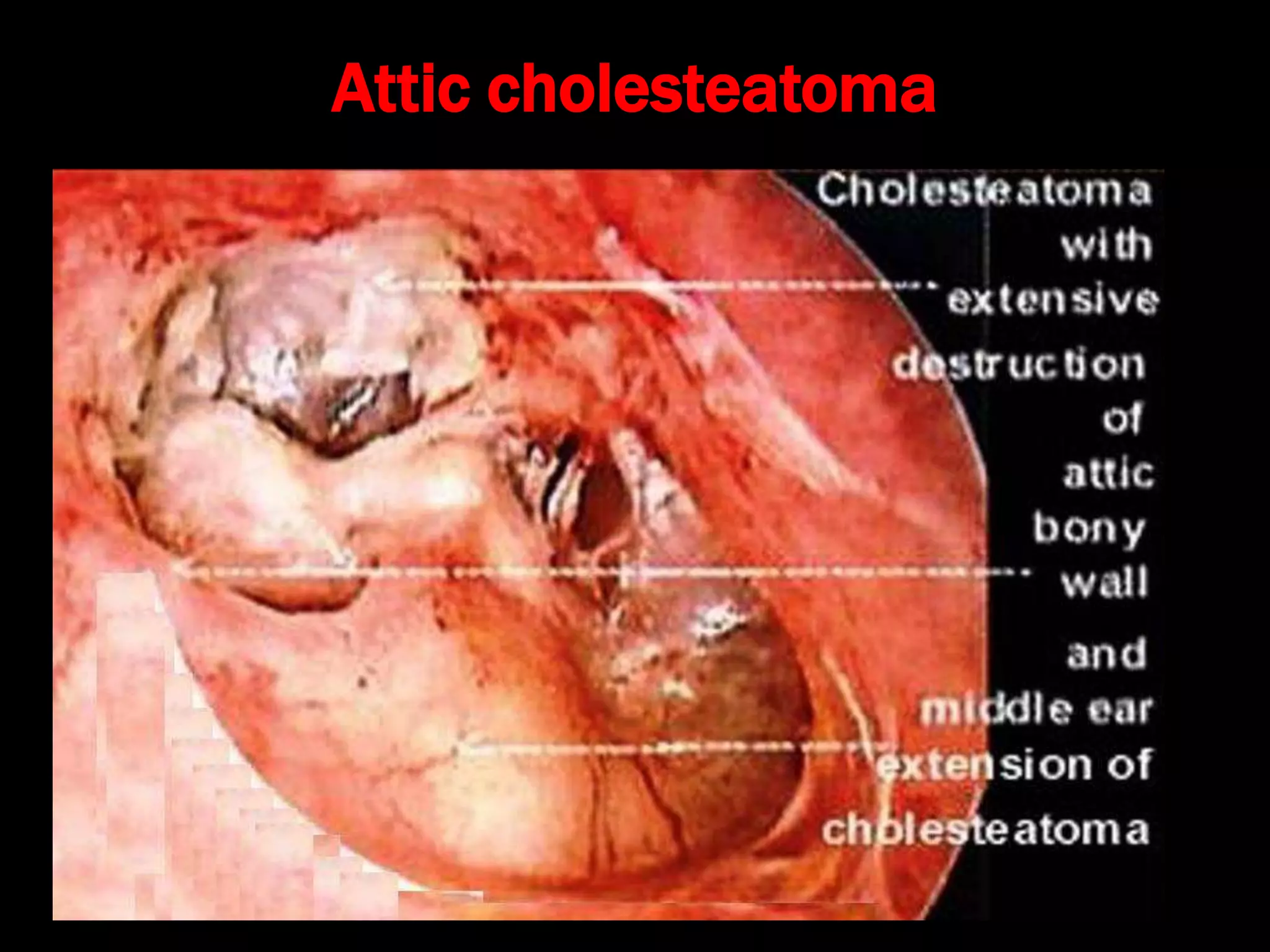
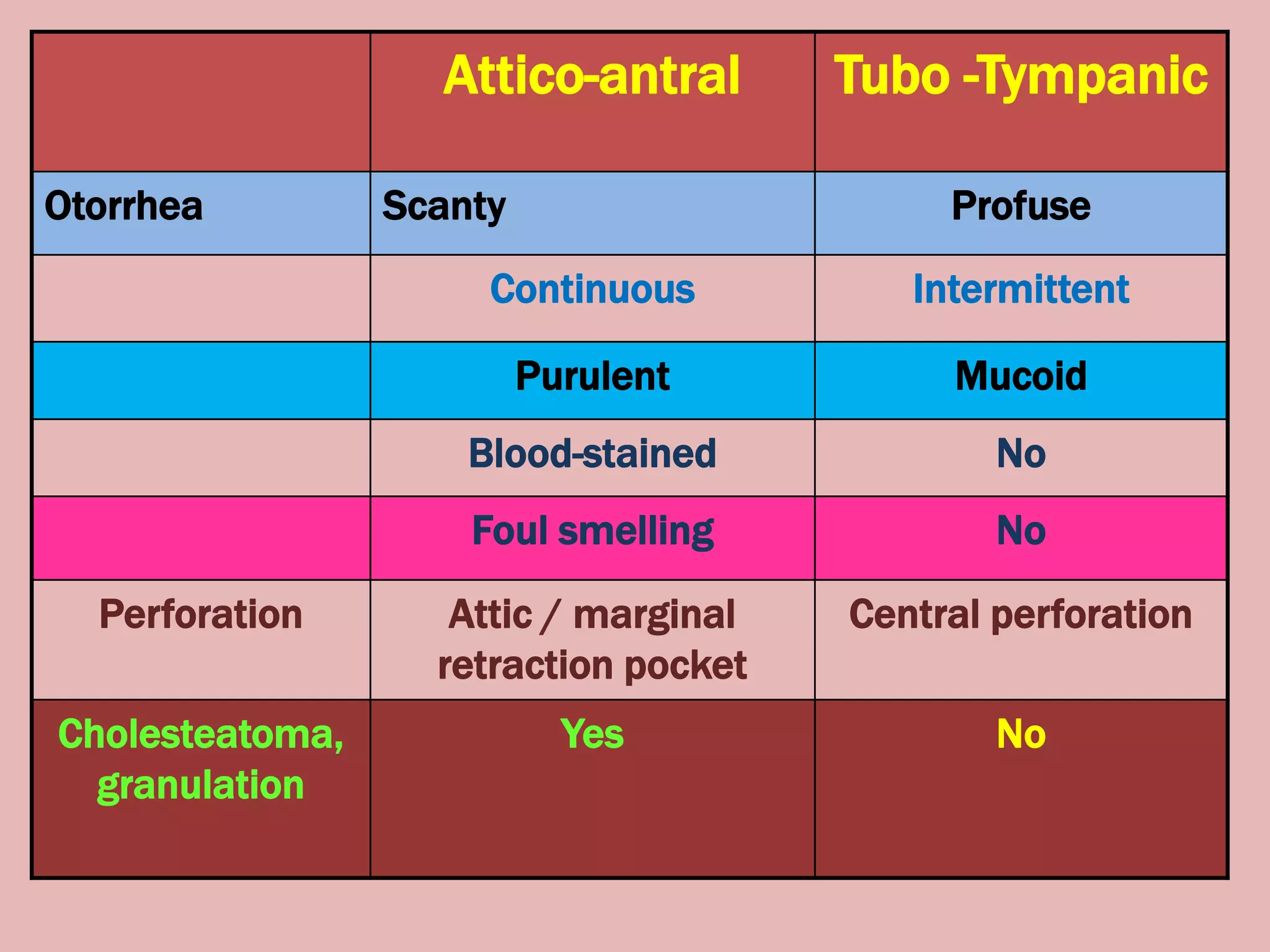
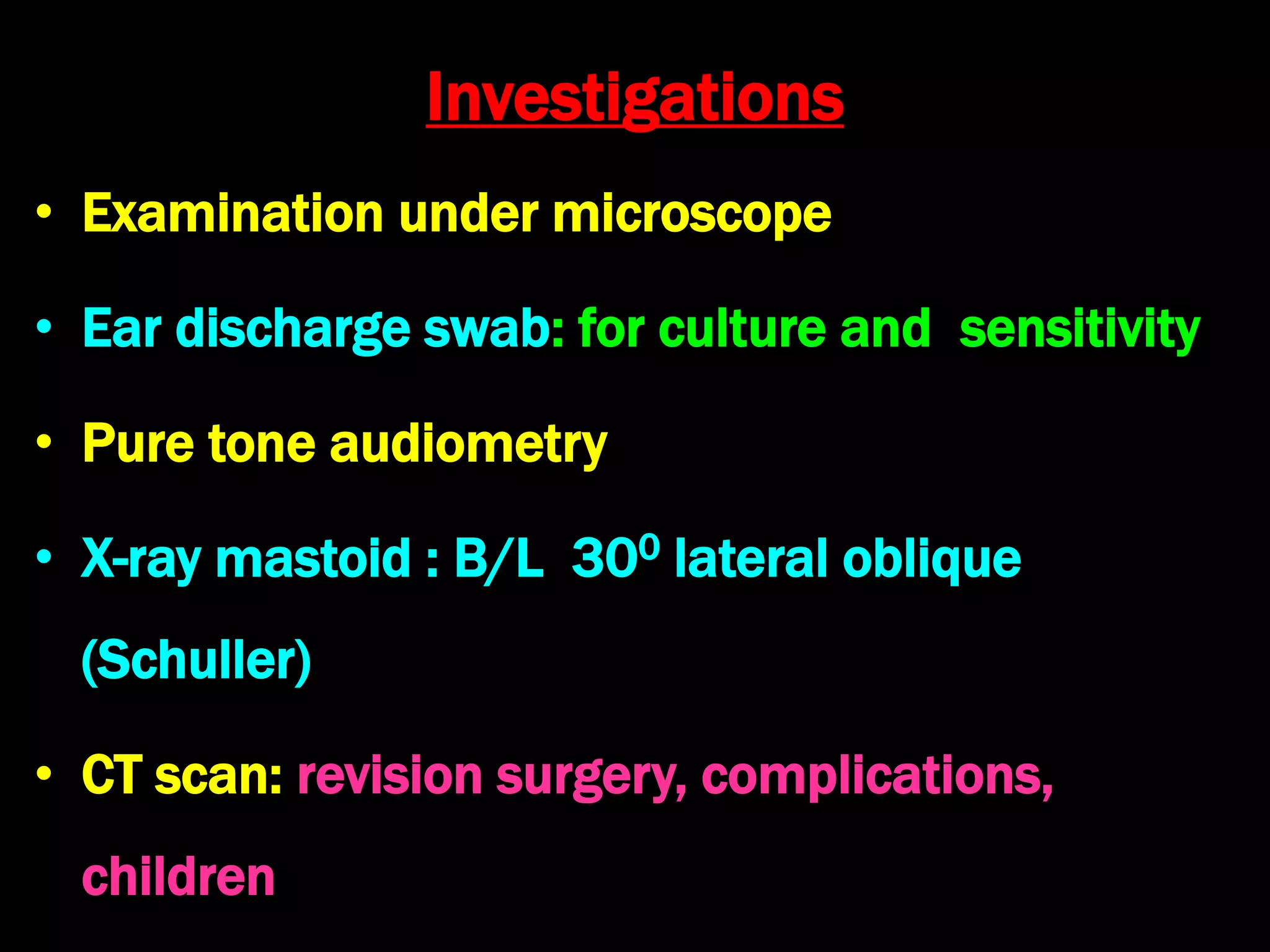
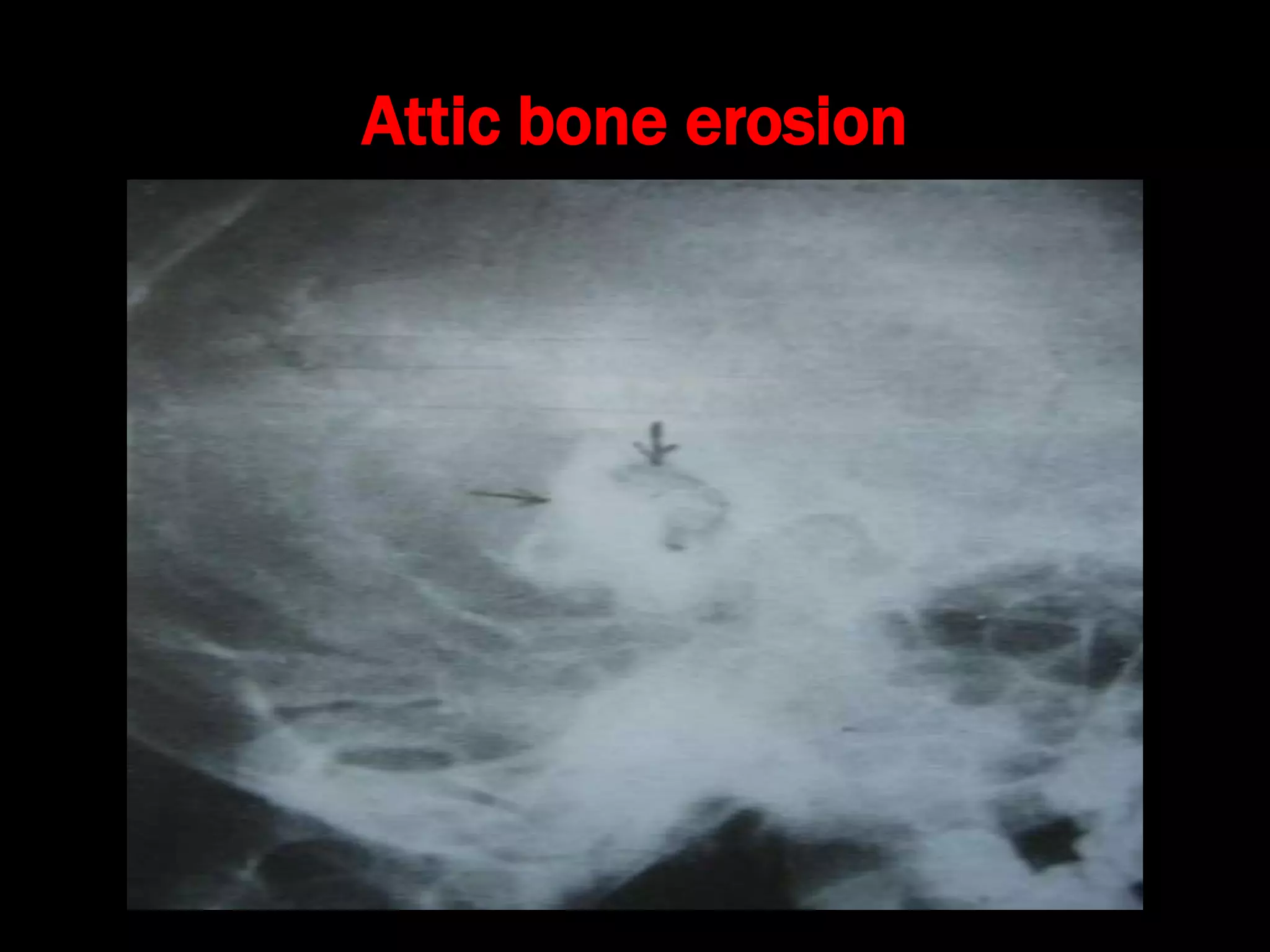
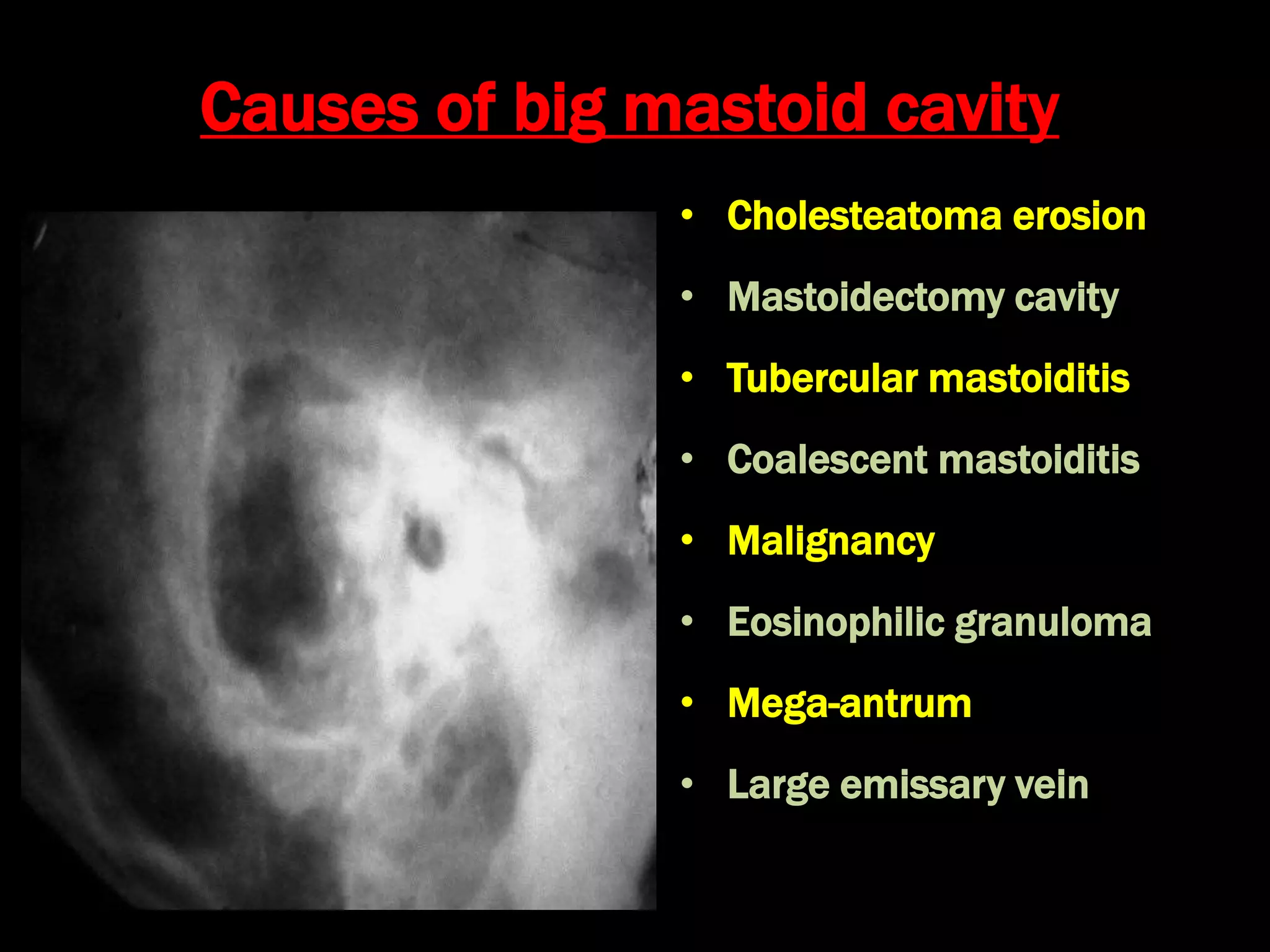
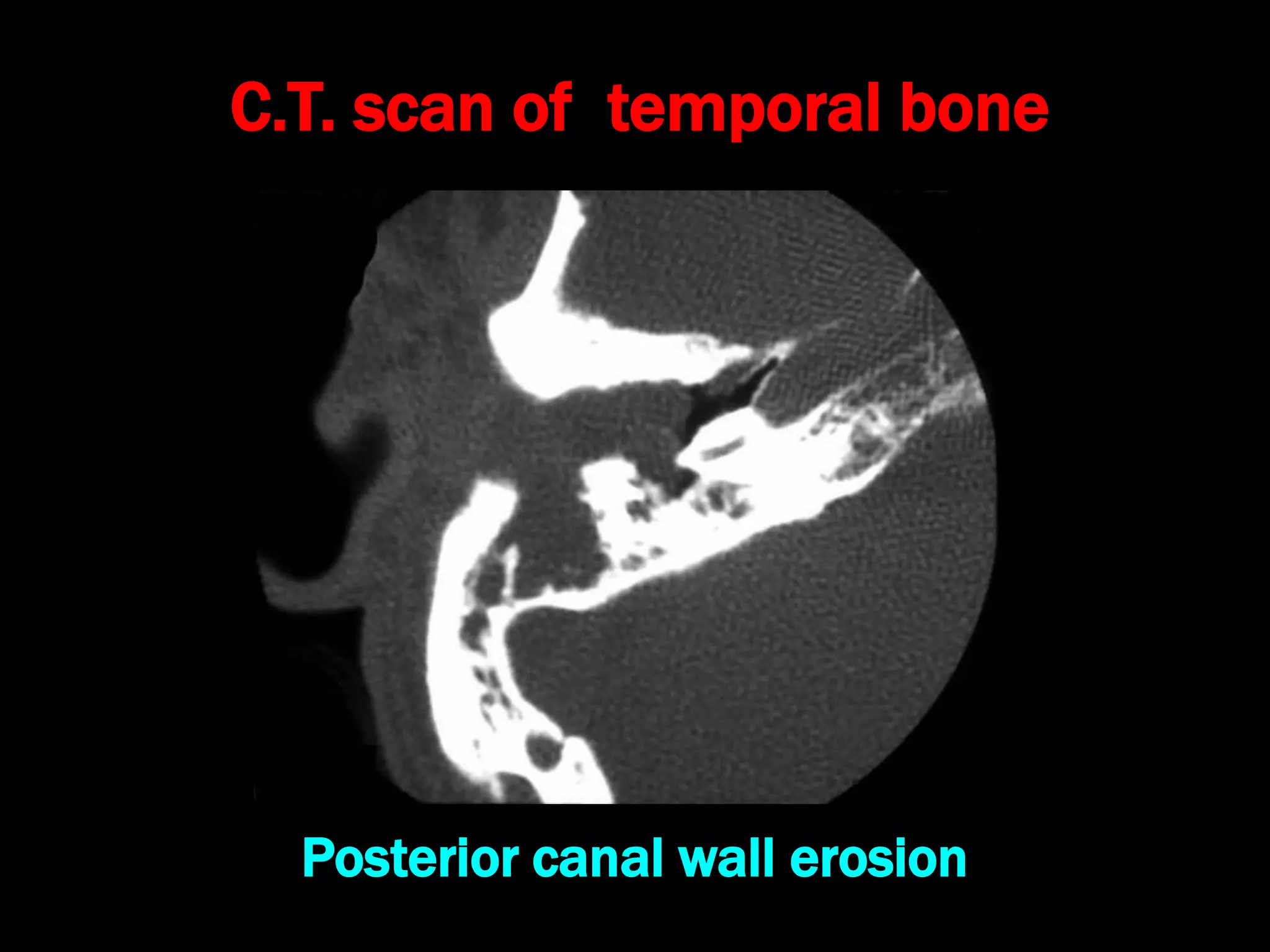
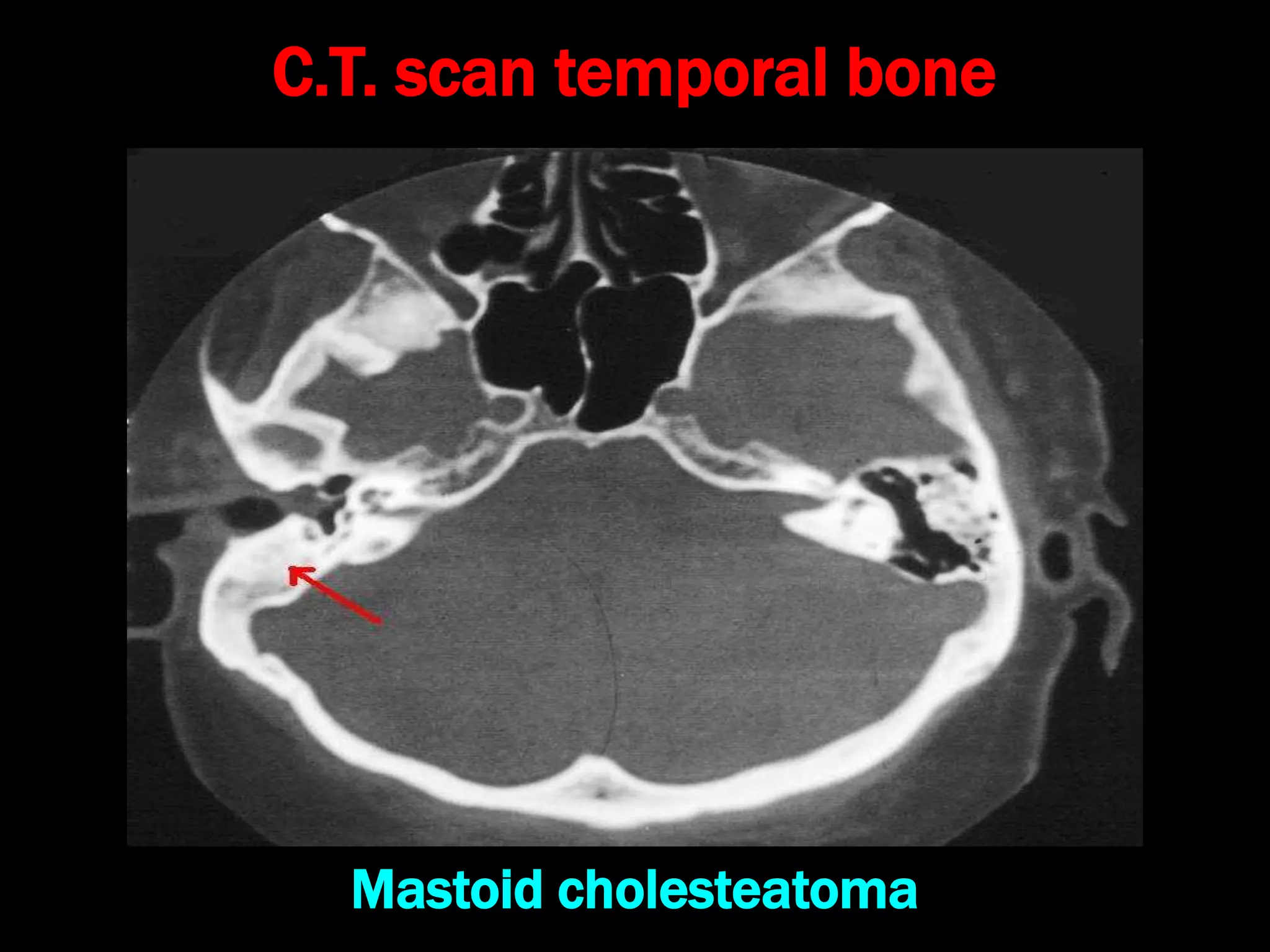
Chronic Suppurative Otitis Media with attico-antral disease (CSOM-AAD), also known as COM-Squamous, is a chronic pyogenic ear infection lasting over 3 months with cholesteatoma and granulation tissue in the attic or posterosuperior quadrant of the eardrum. This causes higher risks of bone erosion and complications. Cholesteatoma is a sac lined with keratinizing squamous epithelium that grows at the expense of surrounding bone. Surgical treatment via canal wall down procedures such as attico-antrostomy or modified/radical mastoidectomy is the mainstay for managing CSOM-AAD and removing chole