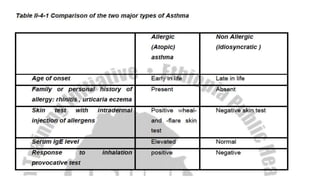
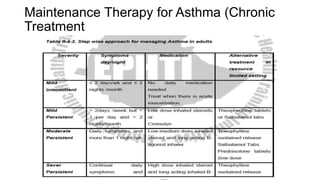
Bronchial asthma is a chronic inflammatory disease of the airways characterized by widespread reversible airway obstruction. It is common, usually starts early in life, and has both genetic and environmental causes like allergens and viruses. Physically, it presents with symptoms like wheezing, coughing, and shortness of breath. Treatment involves bronchodilators, corticosteroids, and avoiding triggers to prevent attacks while chronic maintenance therapy is also needed. Complications can occur if not properly treated.