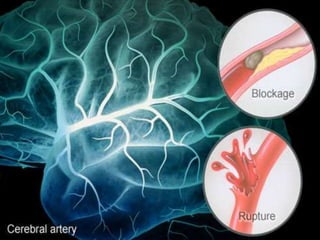
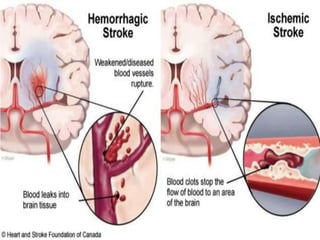
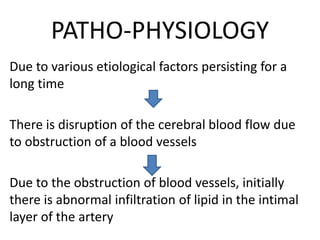
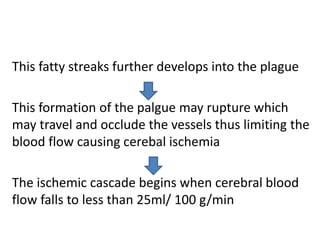
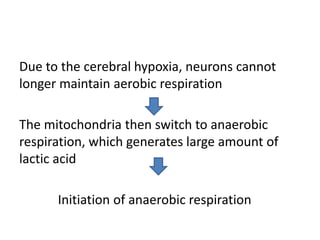
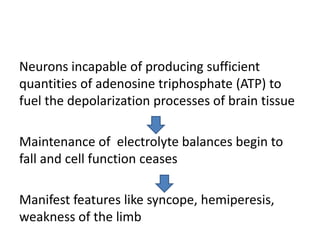
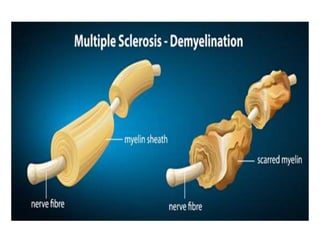
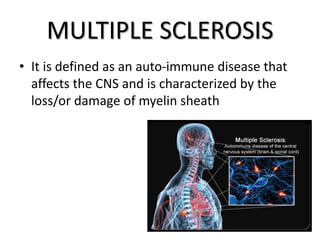
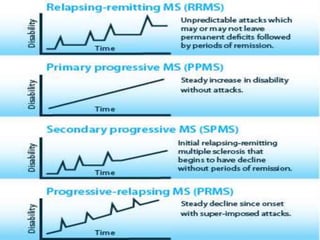
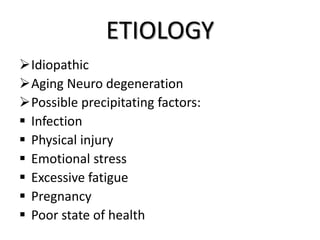
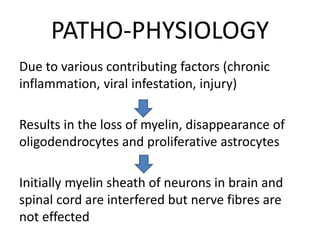
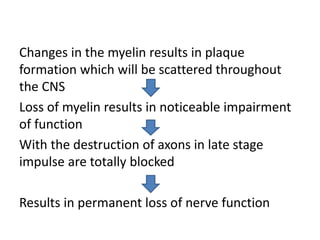
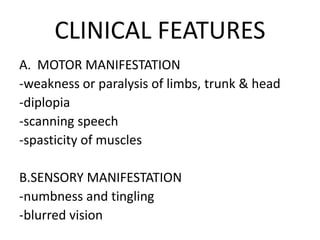
This document discusses stroke and multiple sclerosis. Stroke occurs when there is obstruction of blood flow to the brain or bleeding in the brain, resulting in brain cell death. Risk factors include age, gender, hypertension, heart disease, and smoking. There are two main types of stroke: ischemic and hemorrhagic. Multiple sclerosis is an autoimmune disease characterized by loss of myelin sheath around neurons. There are several types of multiple sclerosis including relapsing-remitting and primary progressive. Management of both conditions involves controlling risk factors, drug therapy like corticosteroids, and surgical procedures for complications.