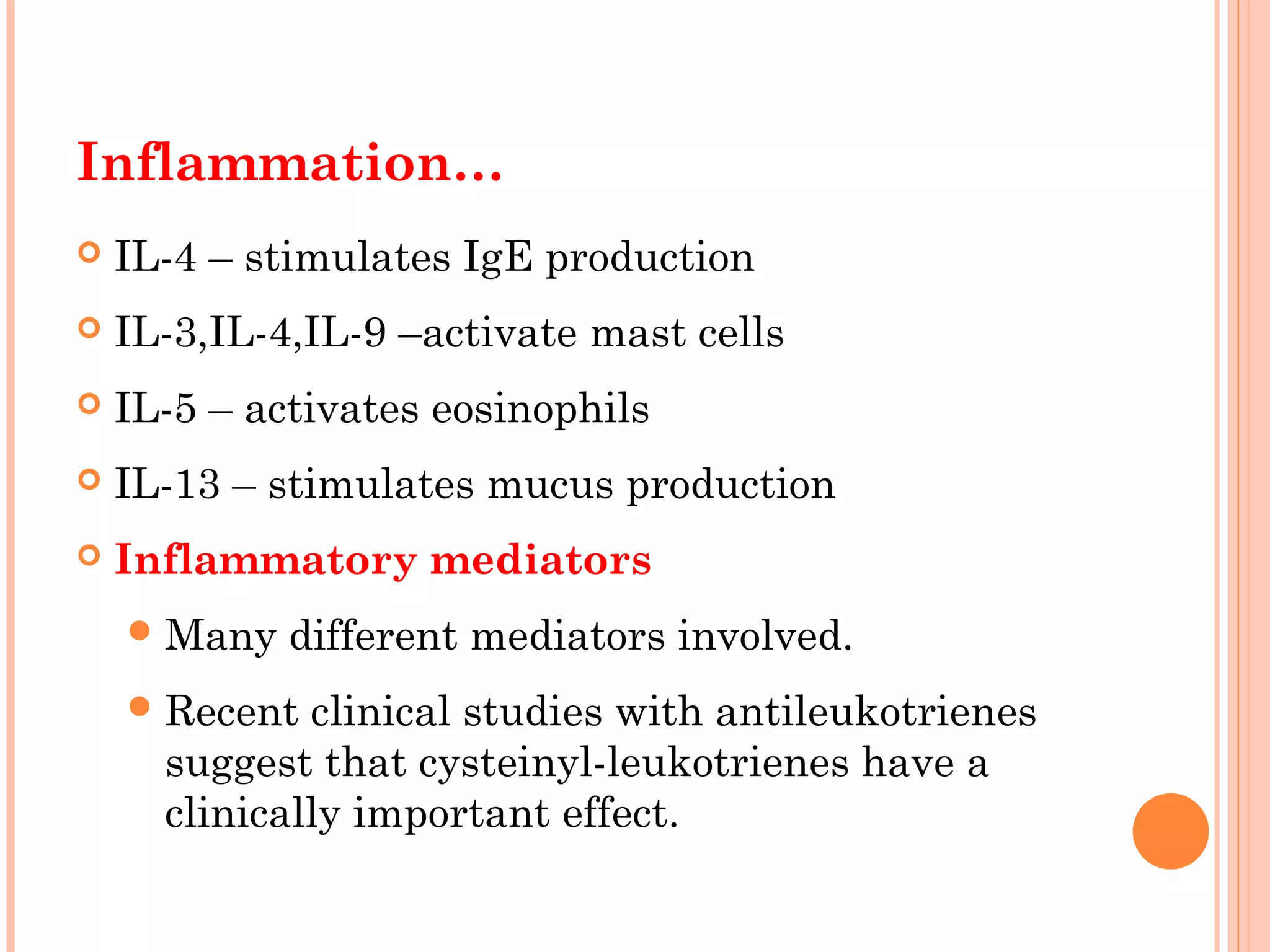
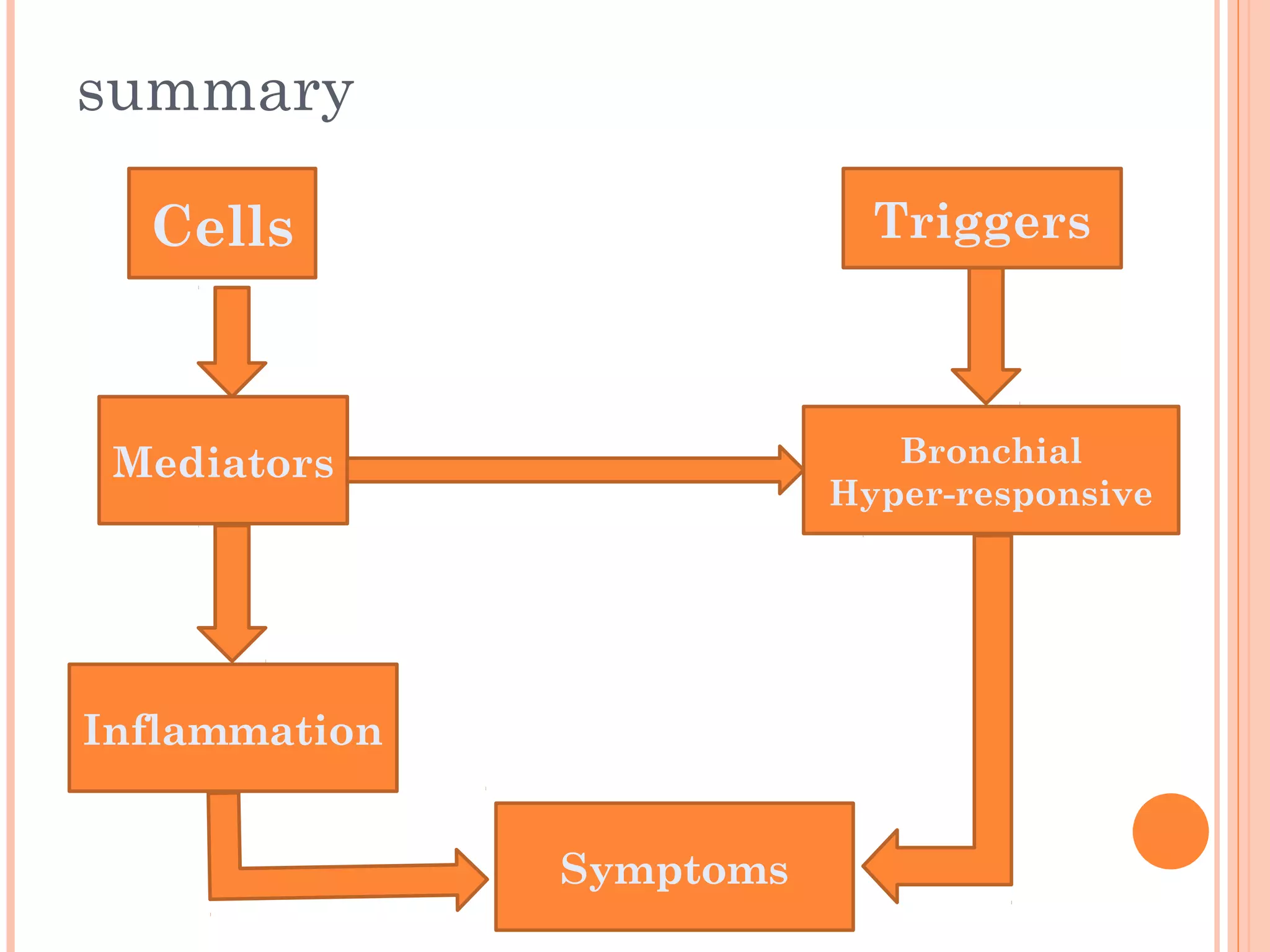
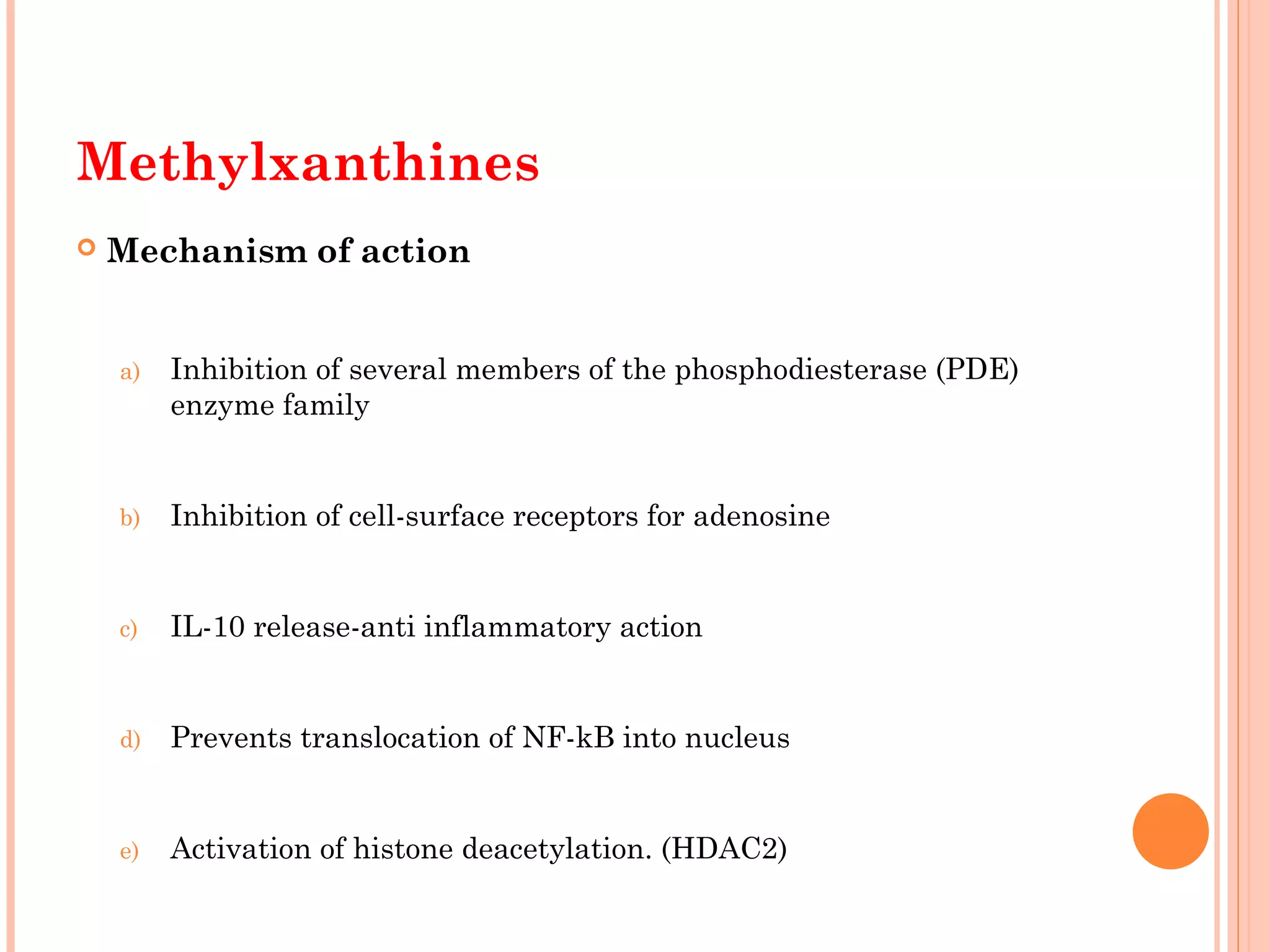
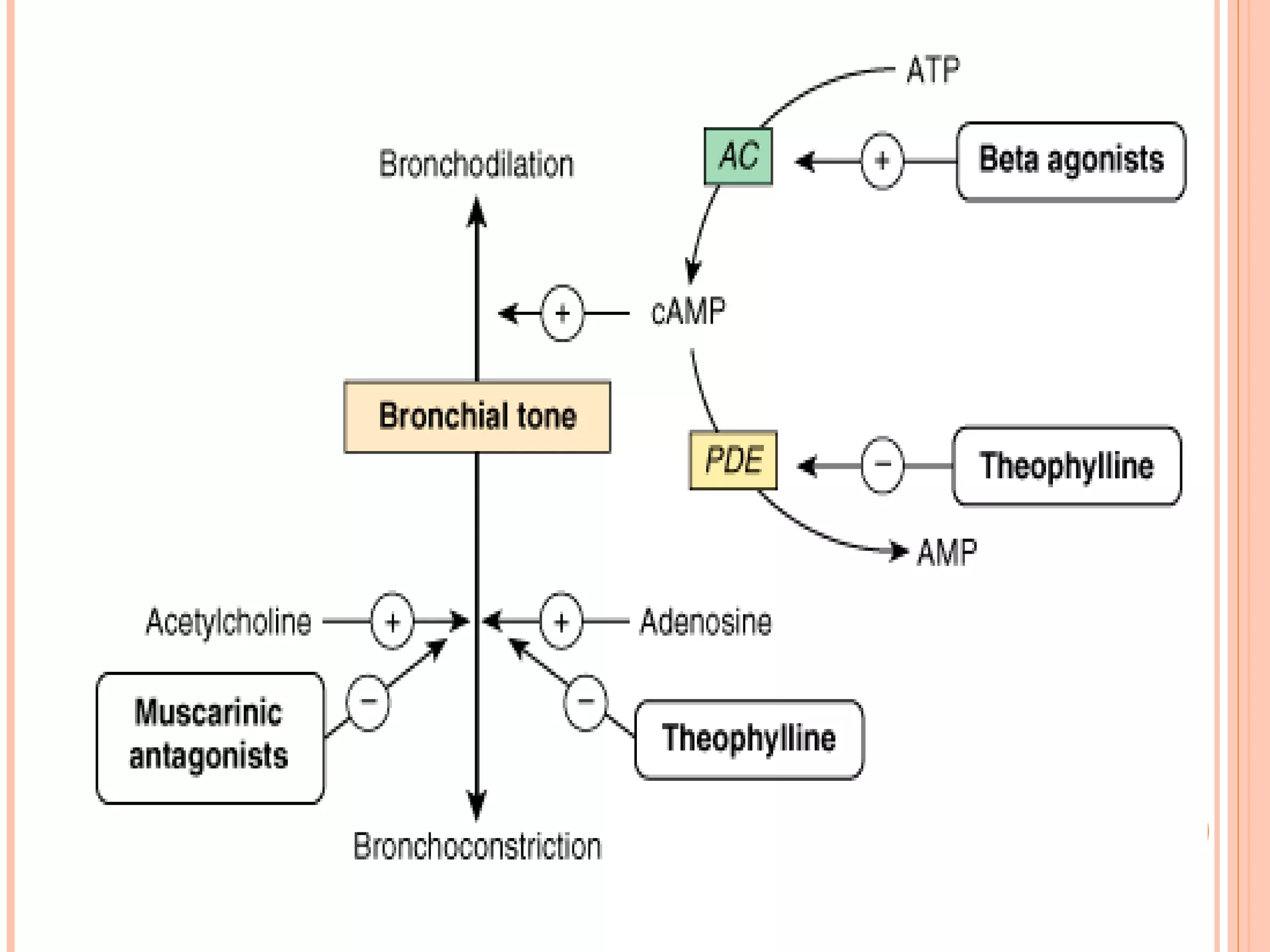
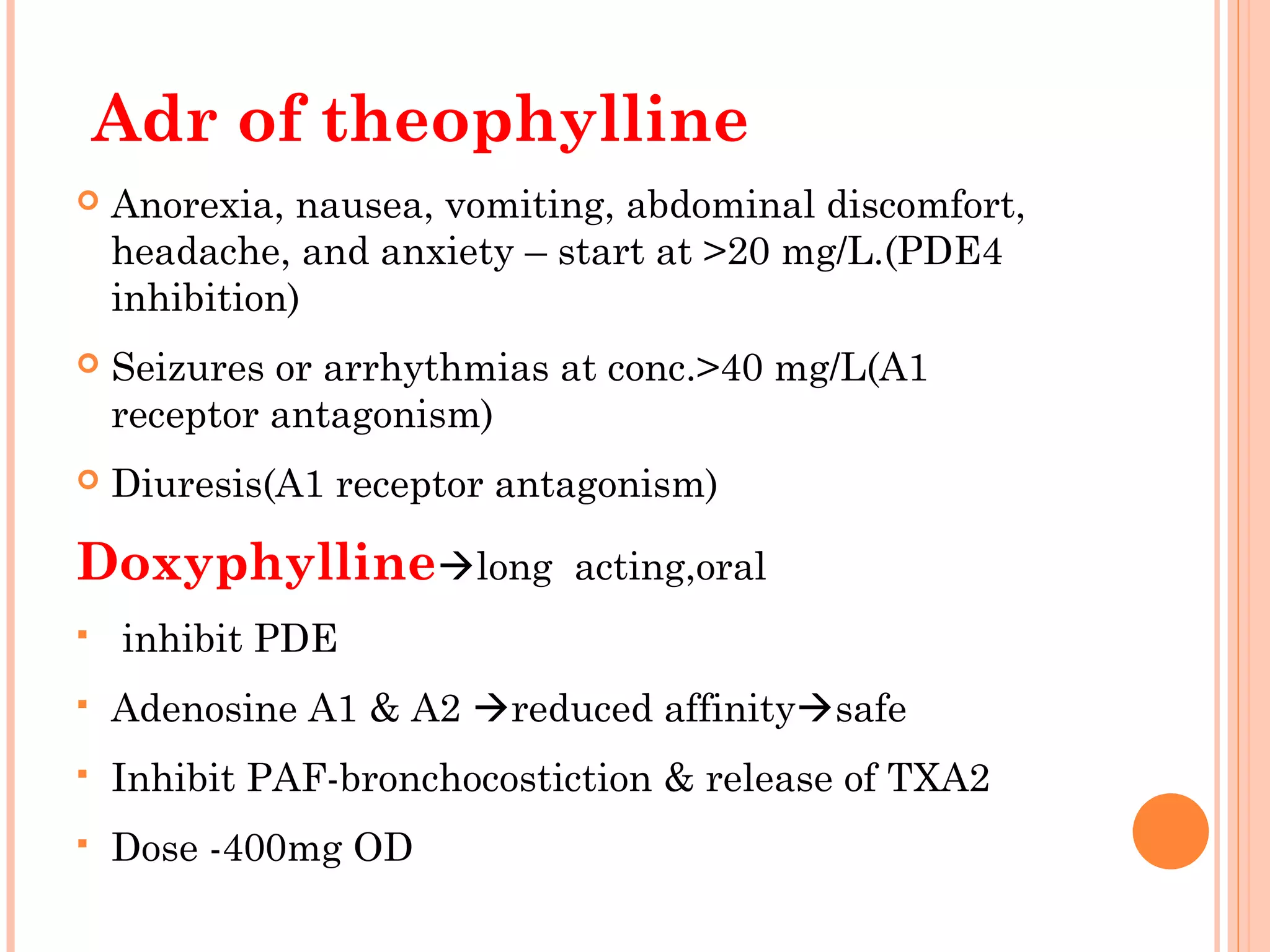
This document provides an overview of the management of bronchial asthma. It discusses the pathophysiology of asthma including chronic airway inflammation and hyperresponsiveness. It describes the clinical presentation of asthma and drug treatments including bronchodilators, corticosteroids, leukotriene inhibitors, and cromones. The document highlights the roles of these drugs in controlling inflammation and reducing exacerbations to manage asthma symptoms.