The document provides information on the medical management of asthma. It outlines the goals of treatment as allowing normal life and decreasing bronchoconstriction. It describes diagnostic tests that may show abnormalities like reduced lung function. Treatment aims to remove triggers and uses medications like bronchodilators, corticosteroids, and leukotriene modifiers. Nursing interventions focus on proper inhaler technique and addressing diagnoses like ineffective breathing to maintain oxygen levels and educate on treatment plans.
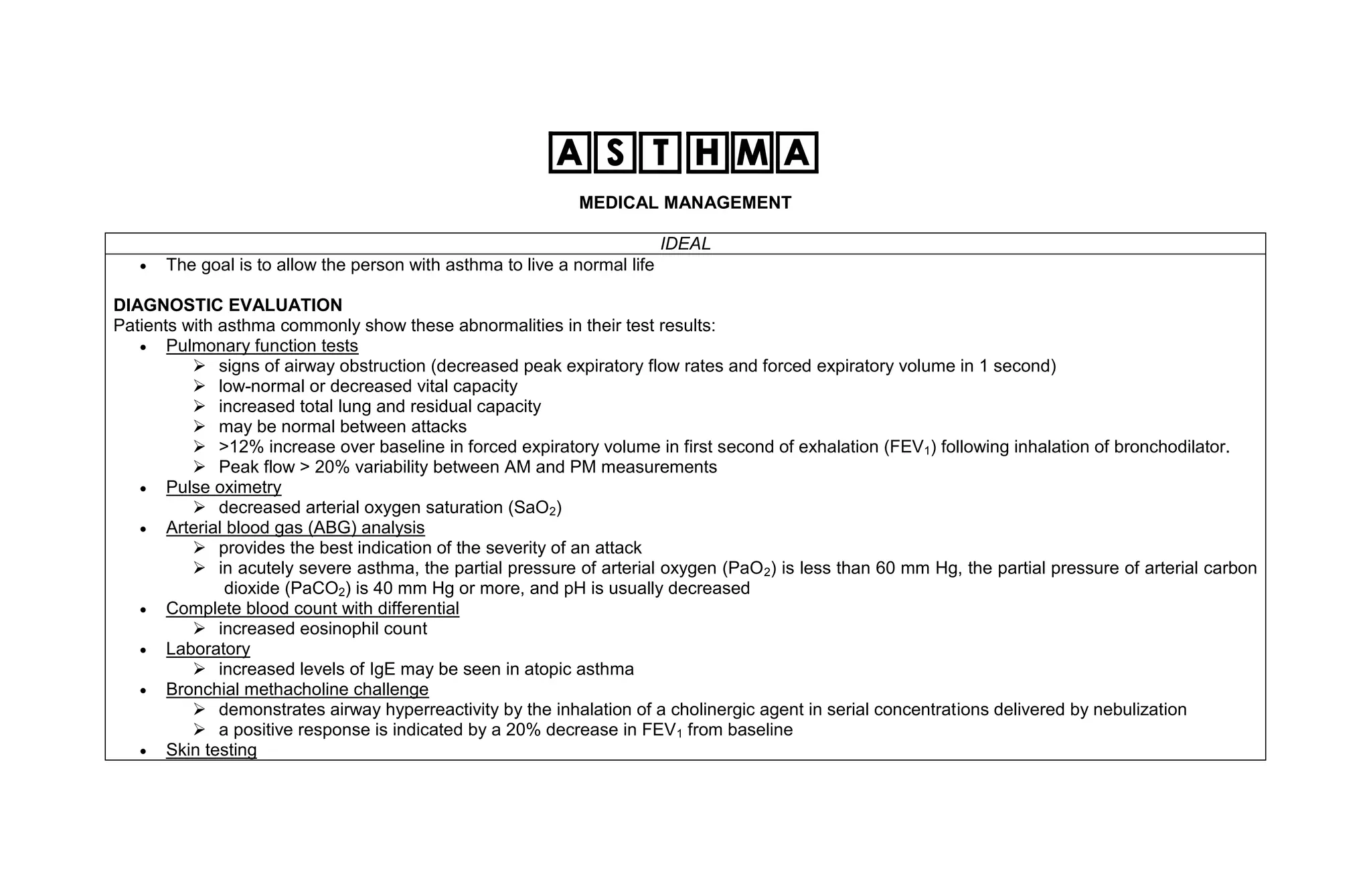

![ Treatment of status asthmaticus consists of aggressive drug therapy:
beta2-adrenergic agonist by nebulizer every 30 to 60 minutes
S.C. epinephrine
I.V. corticosteroid
I.V. aminophylline
oxygen administration
I.V. fluid therapy, and intubation
Mechanical ventilation for hypercapnic respiratory failure (PaCO2 of 40 mm Hg or more).
Quick-relief Medications
Short-acting bronchodilators by inhalation
Beta-agonists, such as albuterol (Proventil, Ventolin), pirbuterol (Maxair), and levalbuterol (Xopenex)
Anticholinergic agent ipratropium bromide (Atrovent)
Systemic corticosteroids (short course)
Long-term Controllers
Inhaled corticosteroids, such as triamcinolone (Azmacort), beclomethasone (Vanceril, Beclovent, QVAR), fluticasone (Flovent), budesonide
(Pulmicort), flunisolide (AeroBid)
Long-acting inhaled beta-agonists include salmeterol (Serevent) and formoterol (Foradil)
Combination inhalers, such as fluticasone and salmeterol (Advair)
Leukotriene modifiers, such as montelukast (Singulair), zafirlukast (Accolate)
Inhaled mast cell stabilizers include cromolyn sodium (Intal) and nedocromil (Tilade)
Long-acting oral beta-agonists such as albuterol extended-release tablets [Volmax])
Oral corticosteroids (maintenance dose)
Methylxanthines such as theophylline (Theo-24, Uniphyl, Theo-Dur)
IgE blocker (omalizumab [Xolair]) can be added to standard maintenance therapy to reduce exacerbations
o subcutaneous injection every 2 to 4 weeks
o The most common adverse reactions are injection site reactions and viral infection
Other Measures
Environmental control](https://image.slidesharecdn.com/asthma-medicalnursingmanagements-110226235349-phpapp01/85/Asthma-medical-nursing-managements-3-320.jpg)





