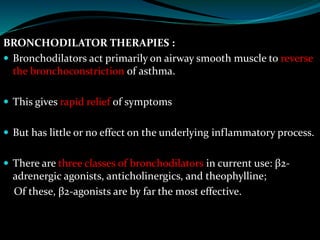
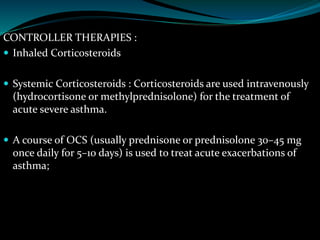
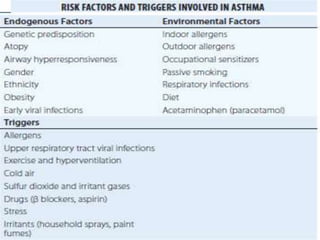
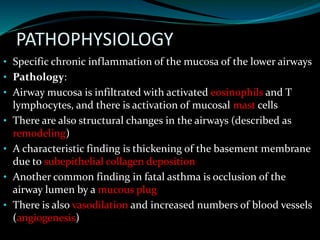
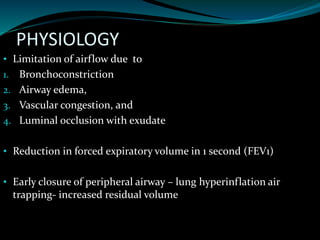
Asthma is characterized by hyperresponsiveness of the airways leading to reversible airflow obstruction and inflammation, with prevalence influenced by genetic, environmental, and atopic factors. It presents variably across ages, with different triggers such as allergens, infections, obesity, and environmental factors exacerbating symptoms. Diagnosis typically involves clinical assessment and lung function tests, while treatment focuses on bronchodilators for immediate relief and corticosteroids to manage inflammation.
![DIAGNOSIS
The diagnosis of asthma is usually done clinically but must be
confirmed by objective measurements of lung function.
Lung Function Tests: Simple spirometry confirms airflow
limitation with a reduced FEV1, FEV1/FVC ratio, and PEF
Hematologic Tests Blood tests are not usually helpful. Total
serum IgE and specific IgE to inhaled allergens
(radioallergosorbent test [RAST]) may be measured in some
patients.](https://image.slidesharecdn.com/asthma-240711084535-e0ca331a/85/ASTHMA-ppt-28-320.jpg)