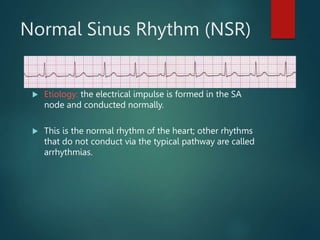
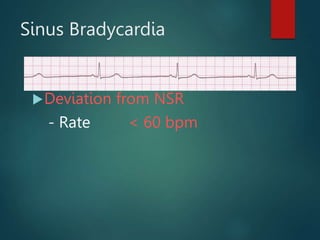
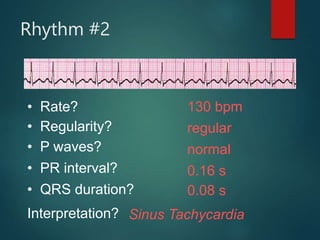
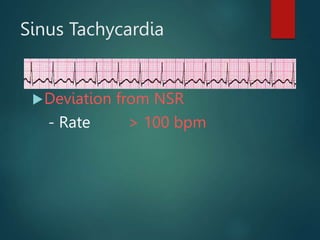
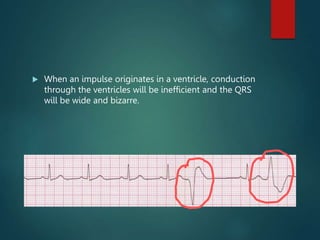
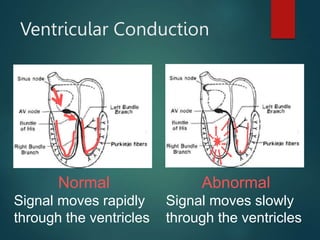
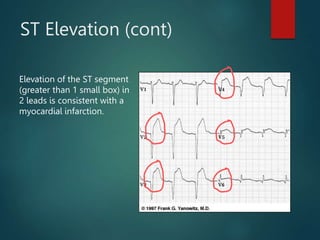
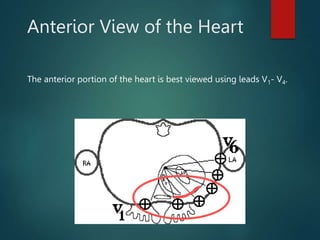
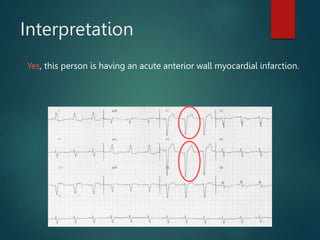
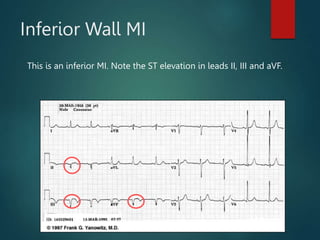
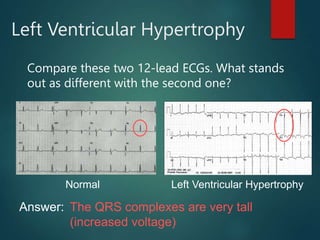
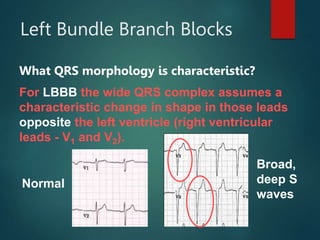
The document provides a comprehensive overview of ECG interpretation, including normal impulse conduction, rhythm analysis, and common arrhythmias. Key sections explain the components of ECG waves, how to calculate heart rates, and assess various heart rhythms leading to conditions like myocardial infarction. It also covers the criteria for diagnosing left ventricular hypertrophy and bundle branch blocks using 12-lead ECGs.