1. Sinus arrhythmia is a normal variation in heart rate due to changes in vagal tone during respiration, causing the P-P interval to vary more than 120 ms in a cyclical fashion.
2. Atrial fibrillation is an irregularly irregular rhythm with no discernible P waves and a variable ventricular rate.
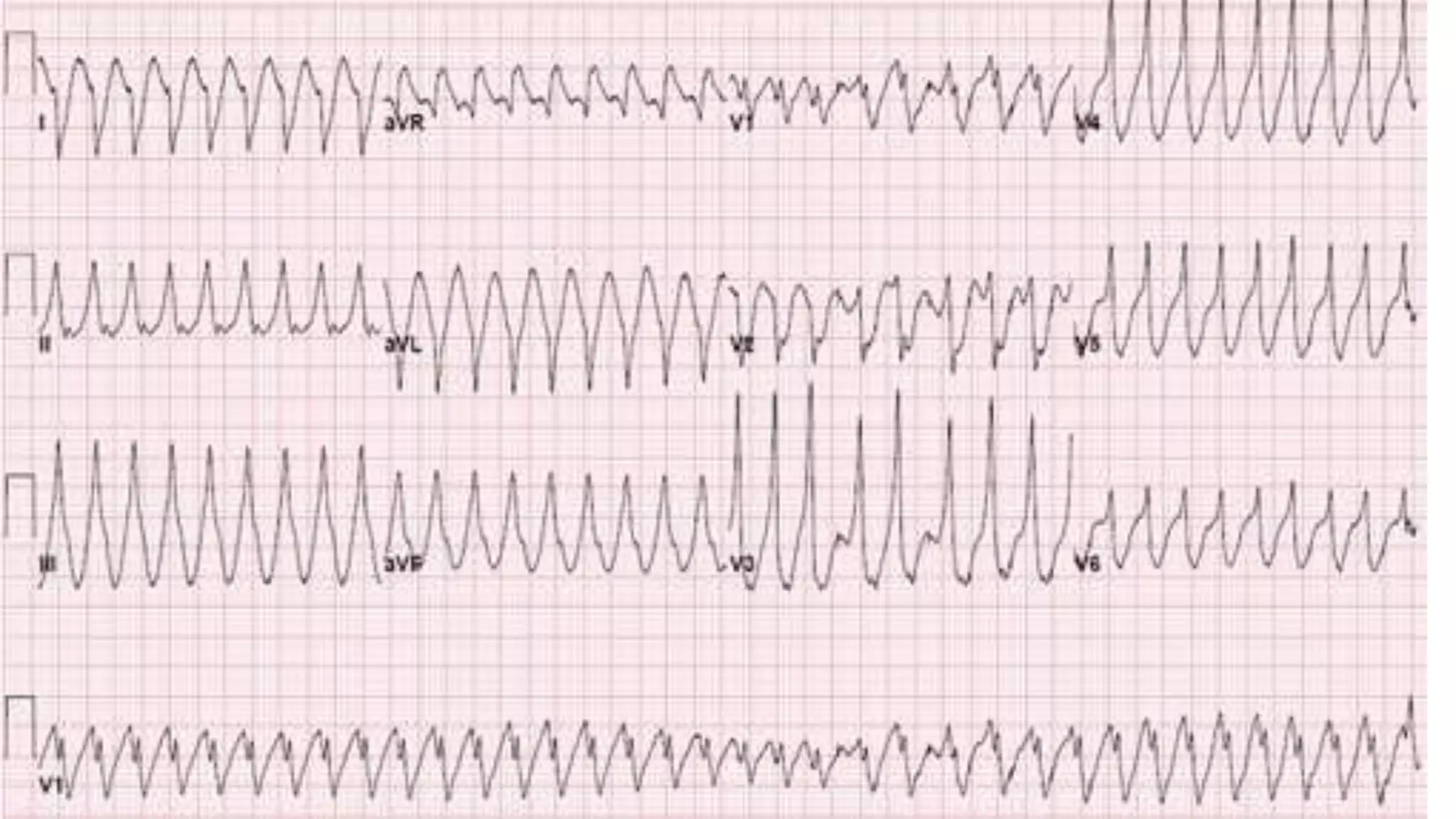
3. Ventricular tachycardia is 3 or more ventricular ectopic beats at a rate over 130 bpm, which can be either monomorphic or polymorphic.