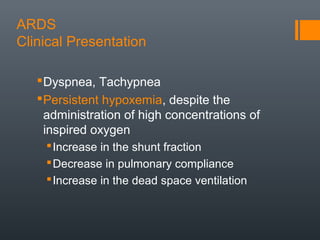
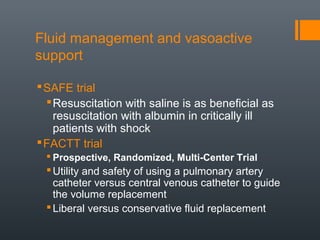
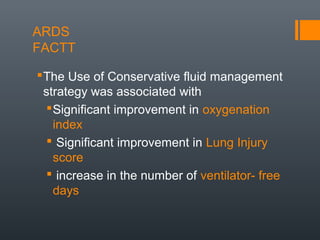
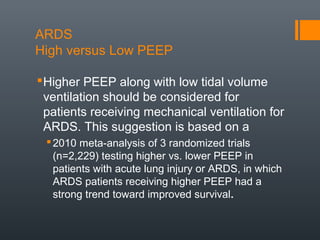
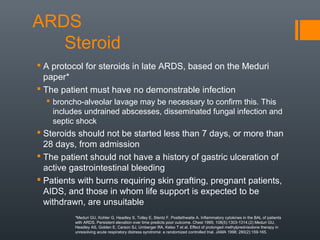
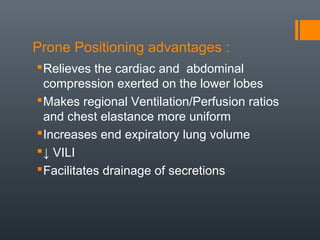
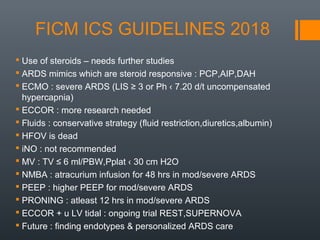
This document discusses acute respiratory distress syndrome (ARDS). It begins with defining ARDS and reviewing its pathophysiology and risk factors. ARDS involves acute inflammation of the alveolar-capillary membrane causing pulmonary edema. Major risk factors include sepsis, trauma, burns, and pneumonia. The document then covers the clinical presentation of ARDS, including dyspnea, hypoxemia, and decreased lung compliance. It reviews guidelines for managing ARDS, such as using low tidal volume ventilation, conservative fluid strategies, and considering prone positioning for moderate to severe cases. Overall treatments aim to protect the lungs from further injury while supporting other vital organ functions.