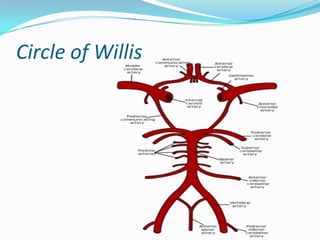
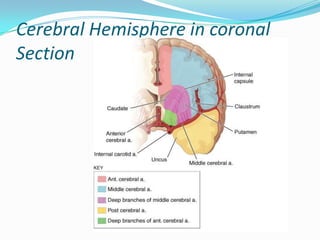
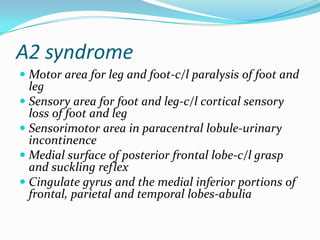
This document provides an overview of stroke syndromes caused by occlusion of arteries in the brain. It describes the classification of strokes as affecting either the anterior or posterior circulation. For anterior circulation strokes, it details the territories supplied and clinical syndromes caused by occlusion of the middle cerebral artery, anterior cerebral artery, and anterior choroidal artery. For posterior circulation strokes, it outlines the arteries involved and syndromes related to vertebral, basilar, and posterior cerebral artery occlusions such as lateral medullary syndrome and lateral pontine syndromes. Diagrams are included to illustrate the vascular anatomy and clinical findings.