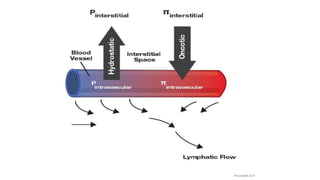
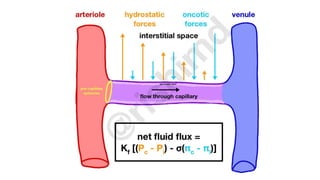
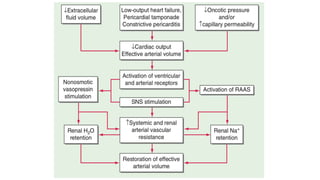
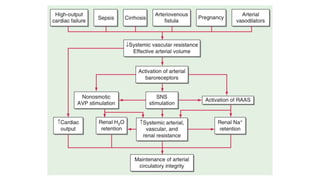
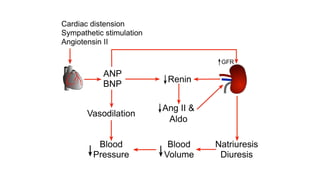
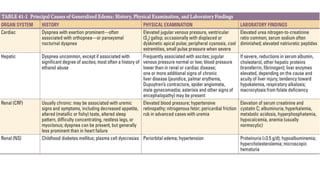
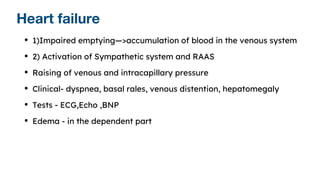
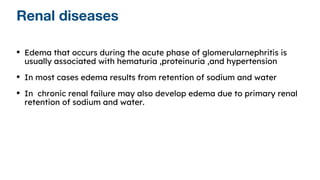
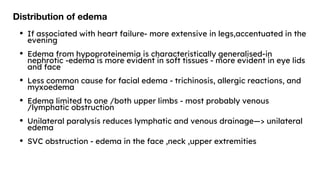
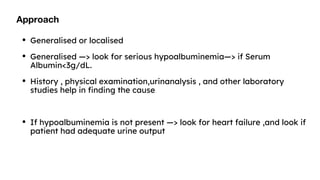
This document discusses edema, including its causes, pathophysiology, and clinical presentations. It defines edema as excess interstitial fluid clinically evident. Edema develops from a net movement of fluid from blood vessels to interstitial space due to increased hydrostatic pressure, impaired lymphatic drainage, decreased oncotic pressure, or capillary damage. Activation of the renin-angiotensin-aldosterone system and arginine vasopressin system can cause sodium and water retention leading to edema. Different diseases like heart failure, renal disease, and liver cirrhosis are discussed in relation to their pathophysiologic mechanisms of edema formation.