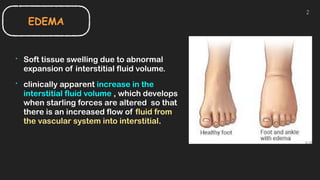
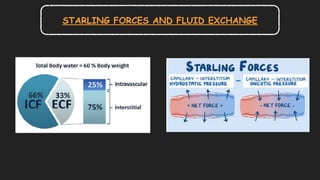
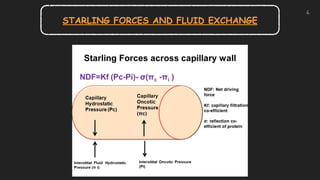
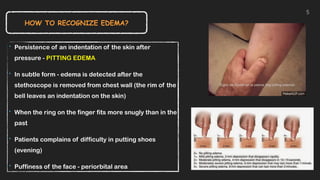
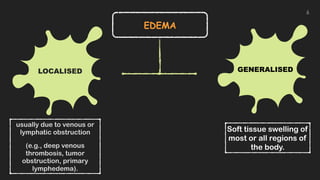
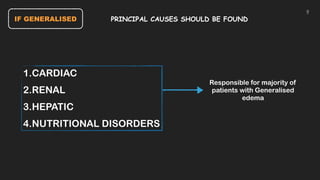
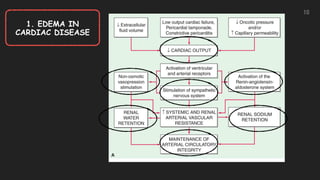
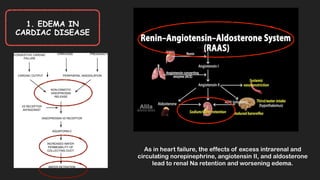
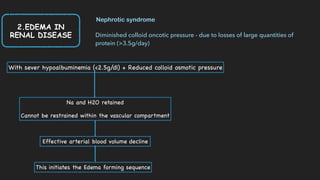
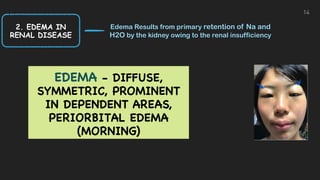
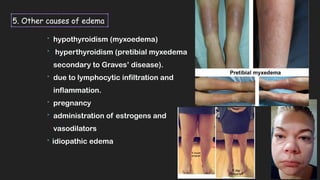
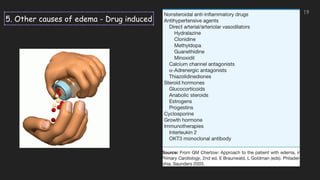
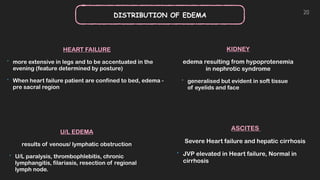
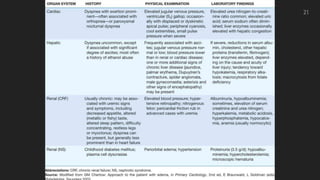
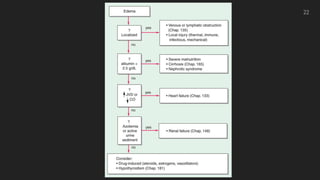
This document discusses the approach to edema. Edema is defined as abnormal soft tissue swelling caused by an increased volume of interstitial fluid. Edema can be localized or generalized depending on its cause. Localized edema is usually due to venous or lymphatic obstruction, while generalized edema can be caused by cardiac, renal, hepatic or nutritional disorders. The causes, signs, and treatments of edema due to these conditions are described. Management involves identifying and treating the underlying cause, restricting sodium and fluid intake, elevating edematous areas, and using compression stockings.