- Edema is an increase in interstitial fluid caused by altered Starling forces that increase fluid flow from blood vessels into tissues.
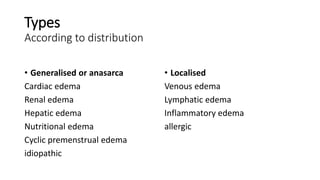
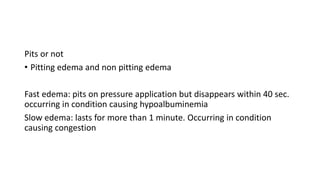
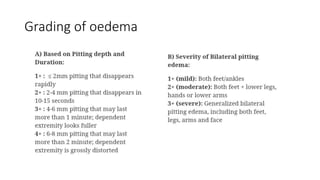
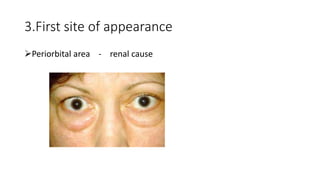
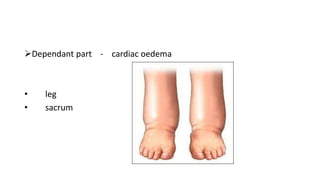
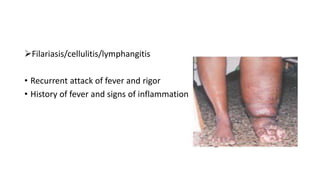
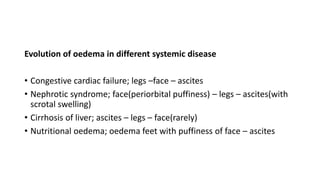
- It can be generalized or localized. Localized edema includes venous, lymphatic, and inflammatory types. Edema can also be pitting or non-pitting.
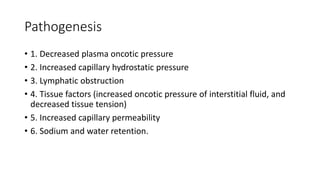
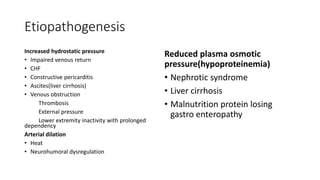
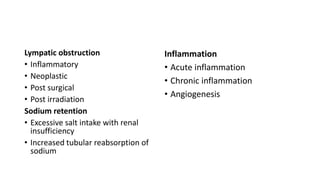
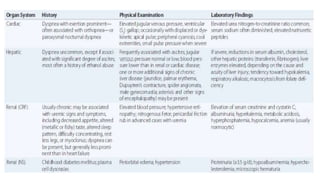
- Common causes of edema include decreased plasma oncotic pressure, increased capillary hydrostatic pressure, lymphatic obstruction, tissue factors, increased capillary permeability, and sodium and water retention.