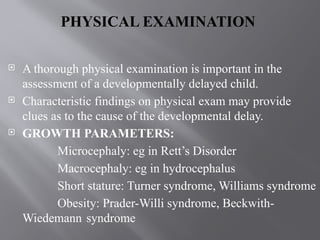
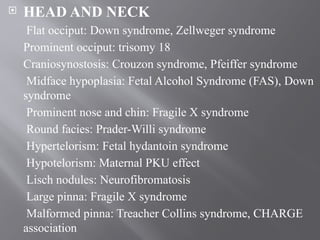
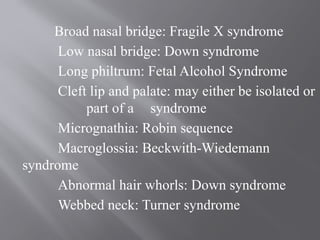
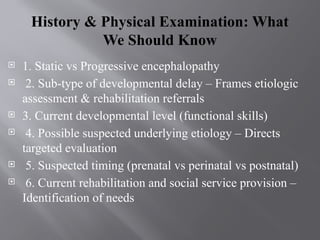
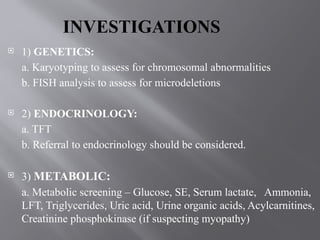
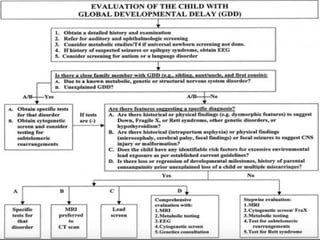
The document discusses the assessment and approach to children with global developmental delay (GDD), emphasizing the importance of early recognition and intervention for optimal developmental outcomes. It outlines various types of developmental delays, assessment techniques, screening tools, and the role of comprehensive evaluation involving different professionals. Additionally, it highlights the need for tailored therapies and early intervention services to support children with GDD and their families.

![ Trivandrum Developmental Screening Test (TDSC) is a
developmental screening test for children. It was
developed by selecting 17 test items from BSID (Baroda
Norms)
It was validated both at the hospital and the community
level against the standard DDST
With a sensitivity of 66.7% and specificity of 78.8%, it can
be used even by community level health worker for mass
screening and takes around 5 minutes to complete.[2]
Includes adequate mental and motor development
milestones spread over the first 2 years.
Requires only a pencil and a bunch of keys as test items.](https://image.slidesharecdn.com/approachtogdd-240904041934-00171a5f/85/Treating-a-Child-with-Global-Developmental-Delay-18-320.jpg)