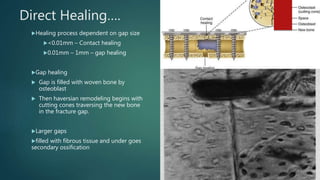
The document provides an overview of fracture healing, detailing biological and mechanical factors that influence the process. It discusses Perren's strain theory, explaining how different levels of interfragmentary strain affect healing pathways, such as direct and indirect healing. Additionally, it covers fixation techniques, factors leading to nonunion, and management strategies for complications like pseudoarthrosis.