1. This document discusses hip fractures, specifically subtrochanteric fractures. It notes that 10-30% of hip fractures are subtrochanteric and they have a bimodal age distribution in those 20-40 years old from high-energy injuries and those over 60 from low-energy falls.
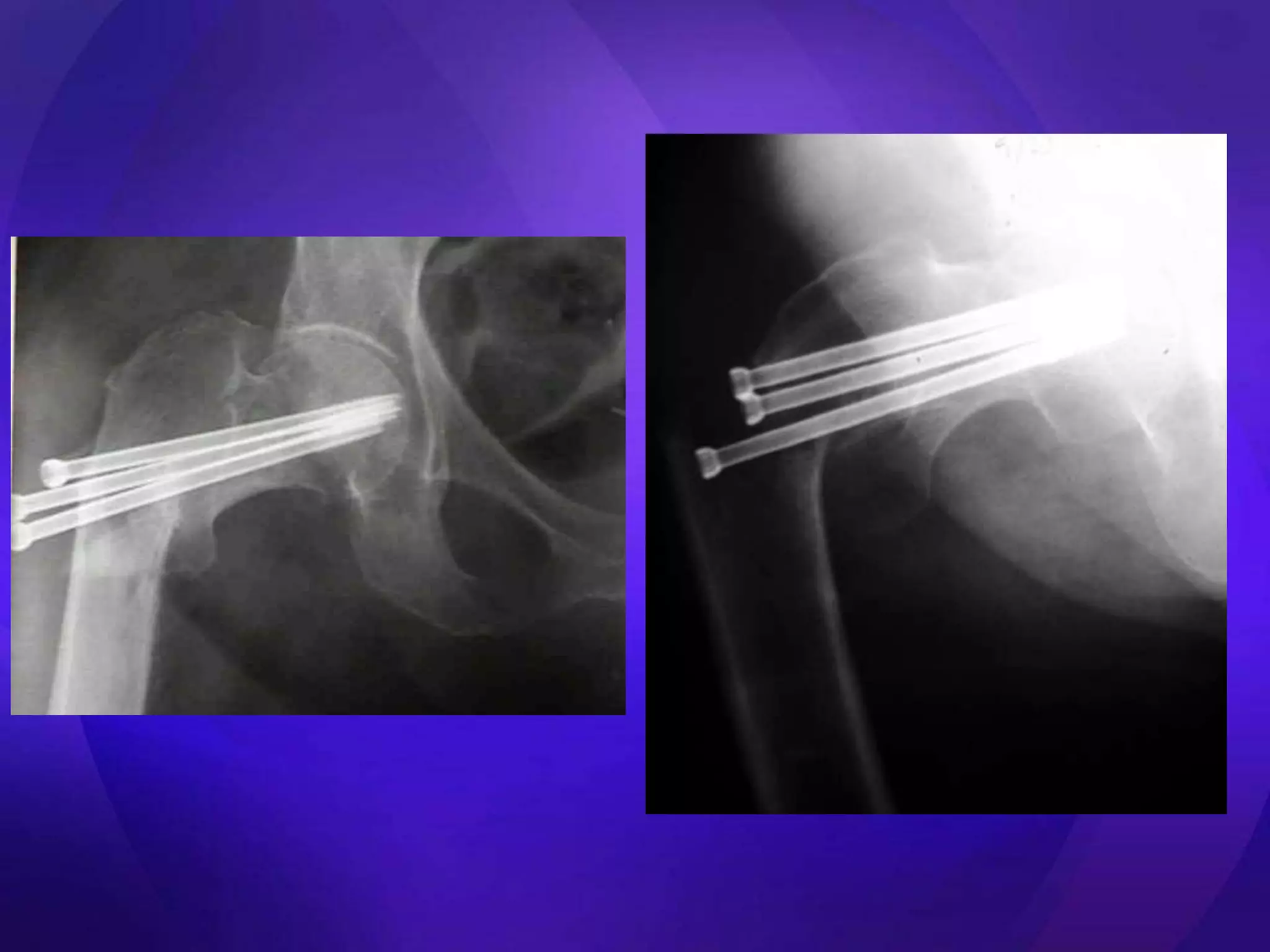
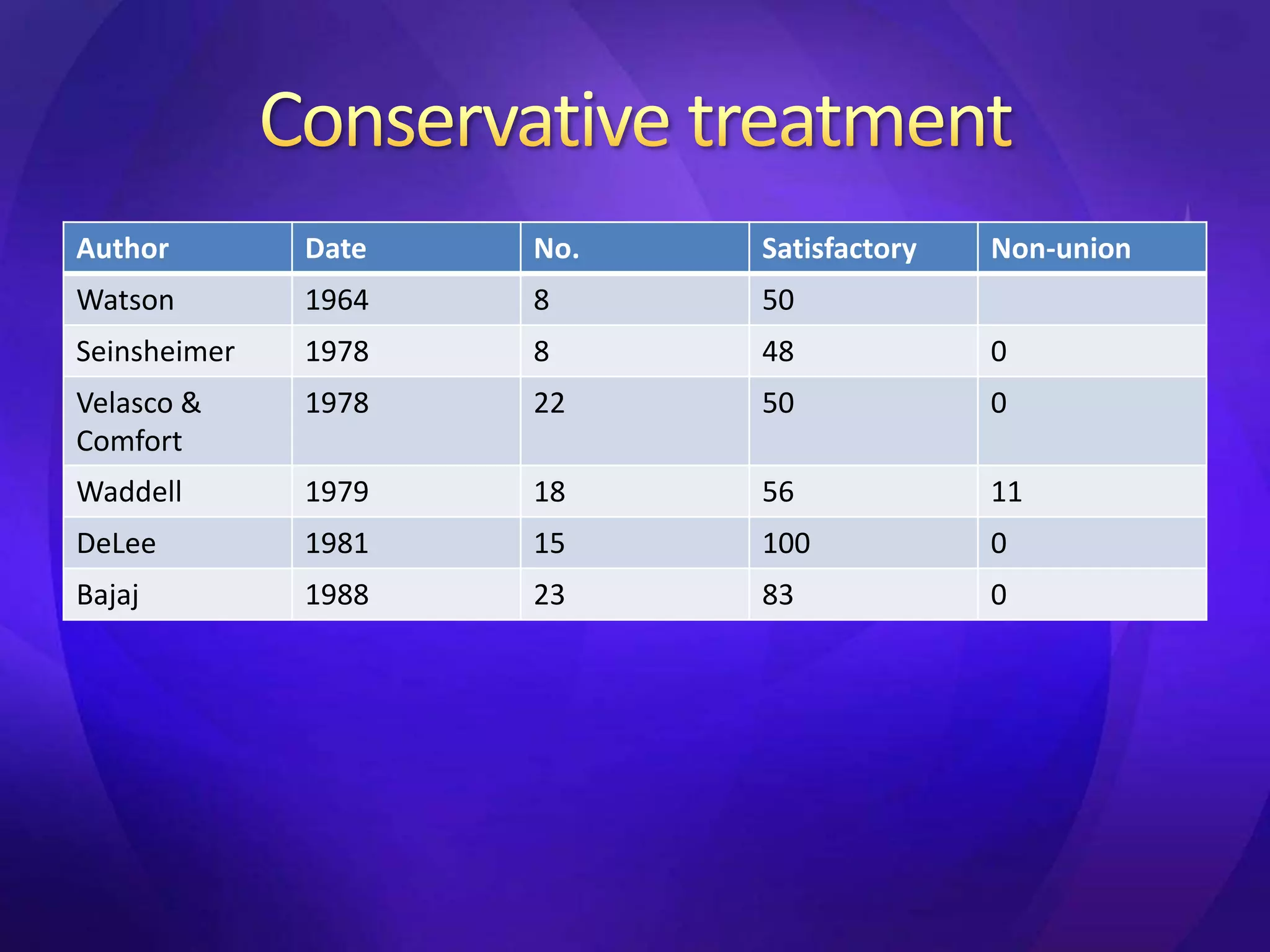
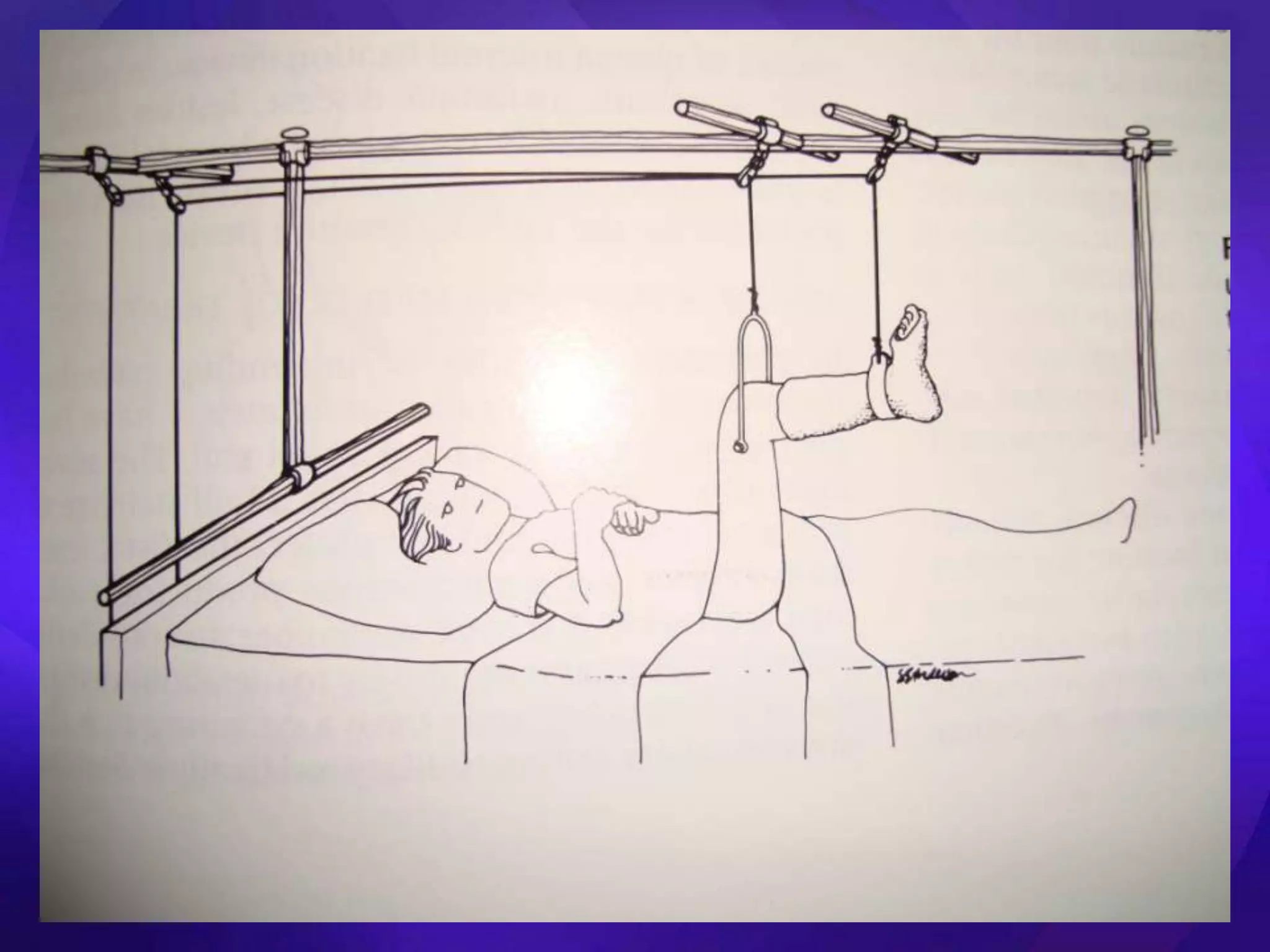
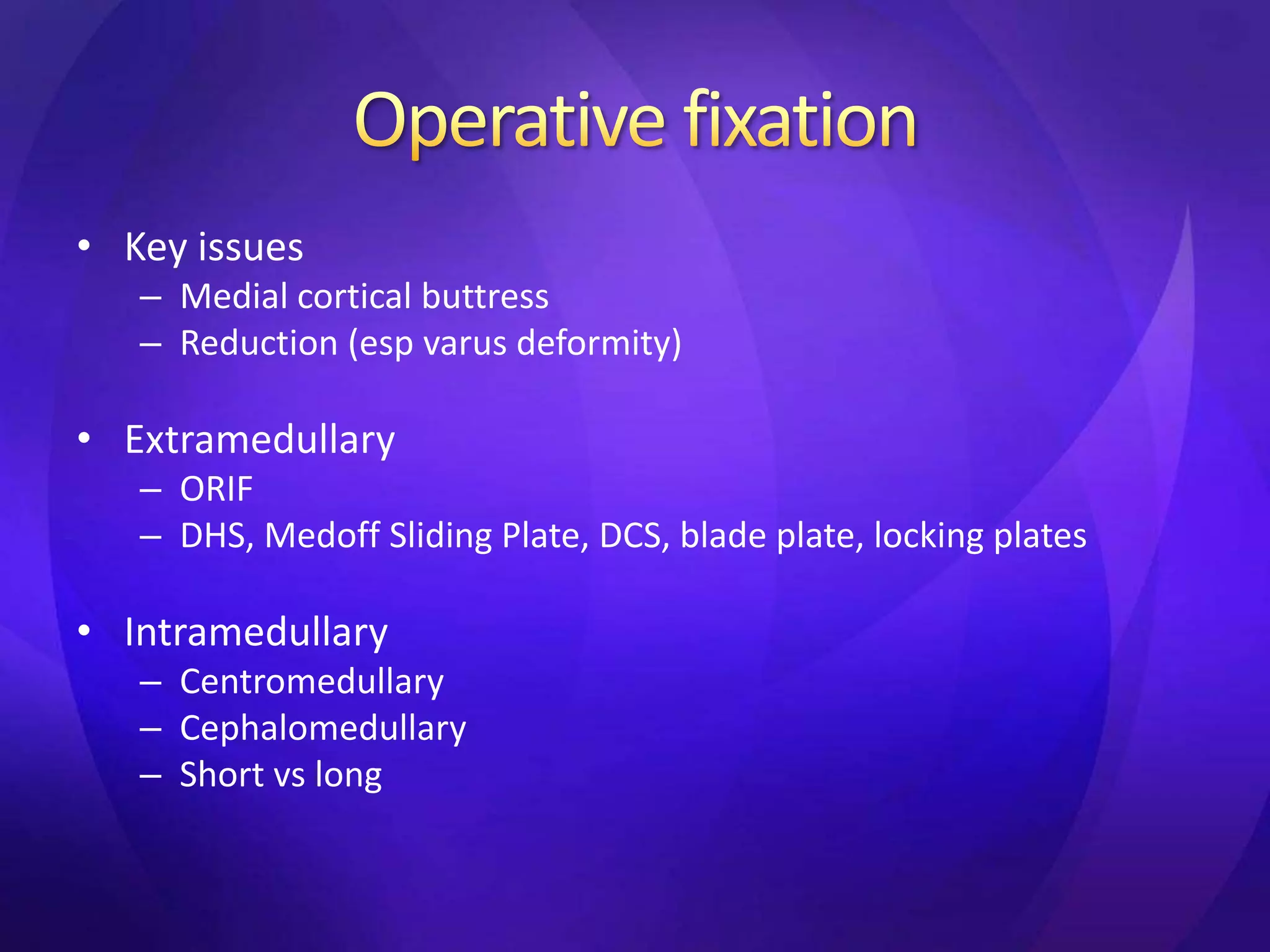
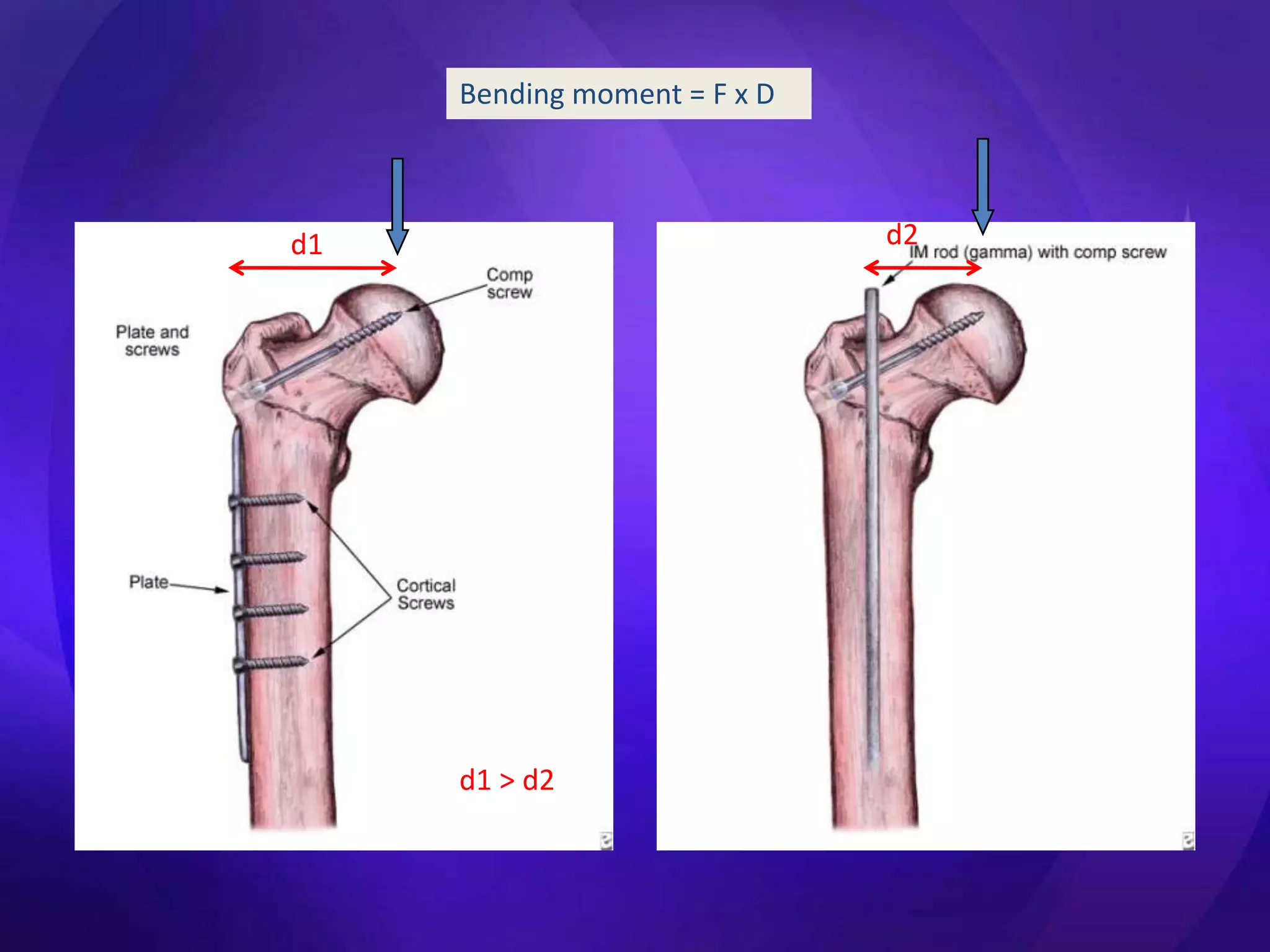
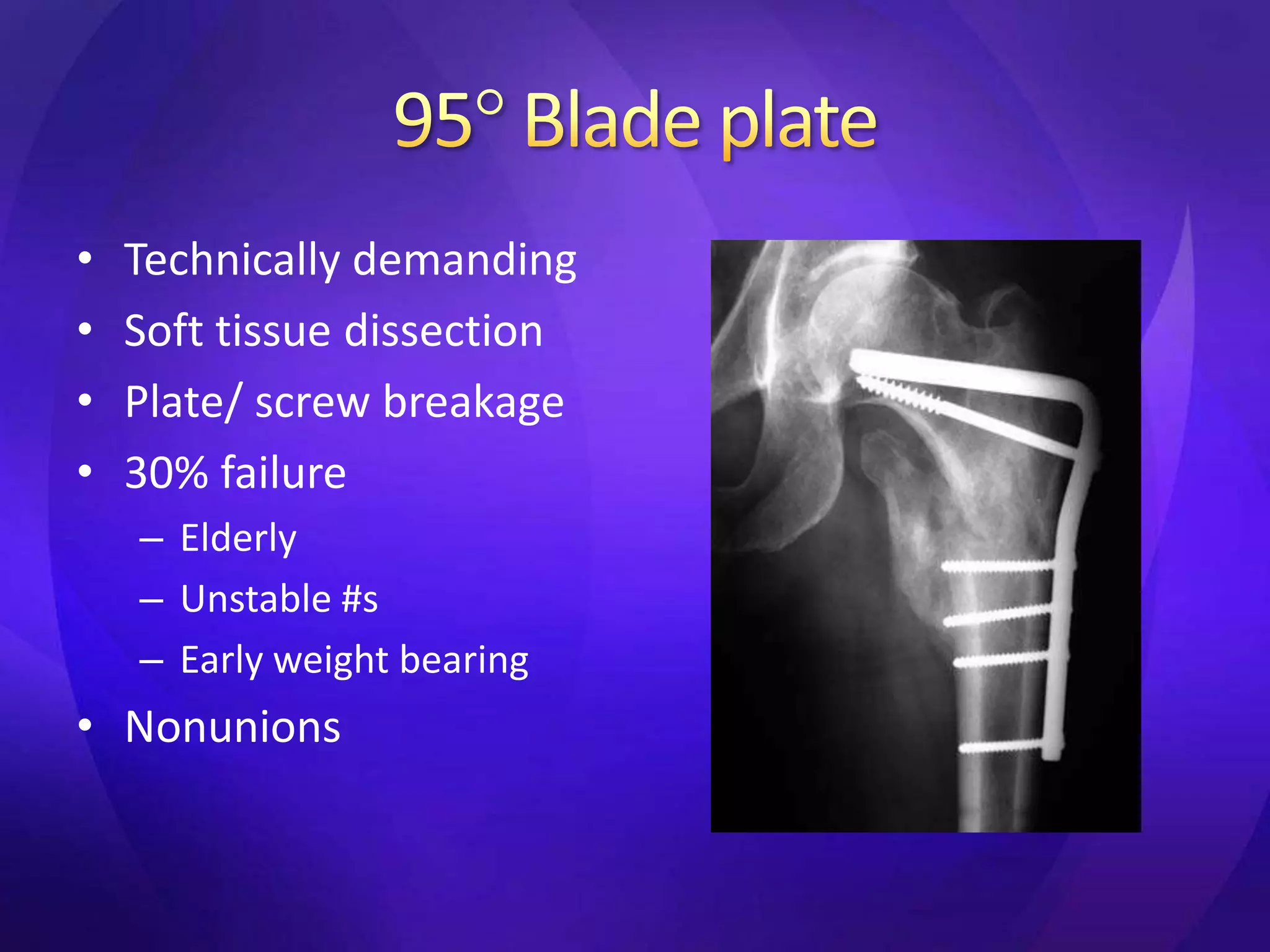
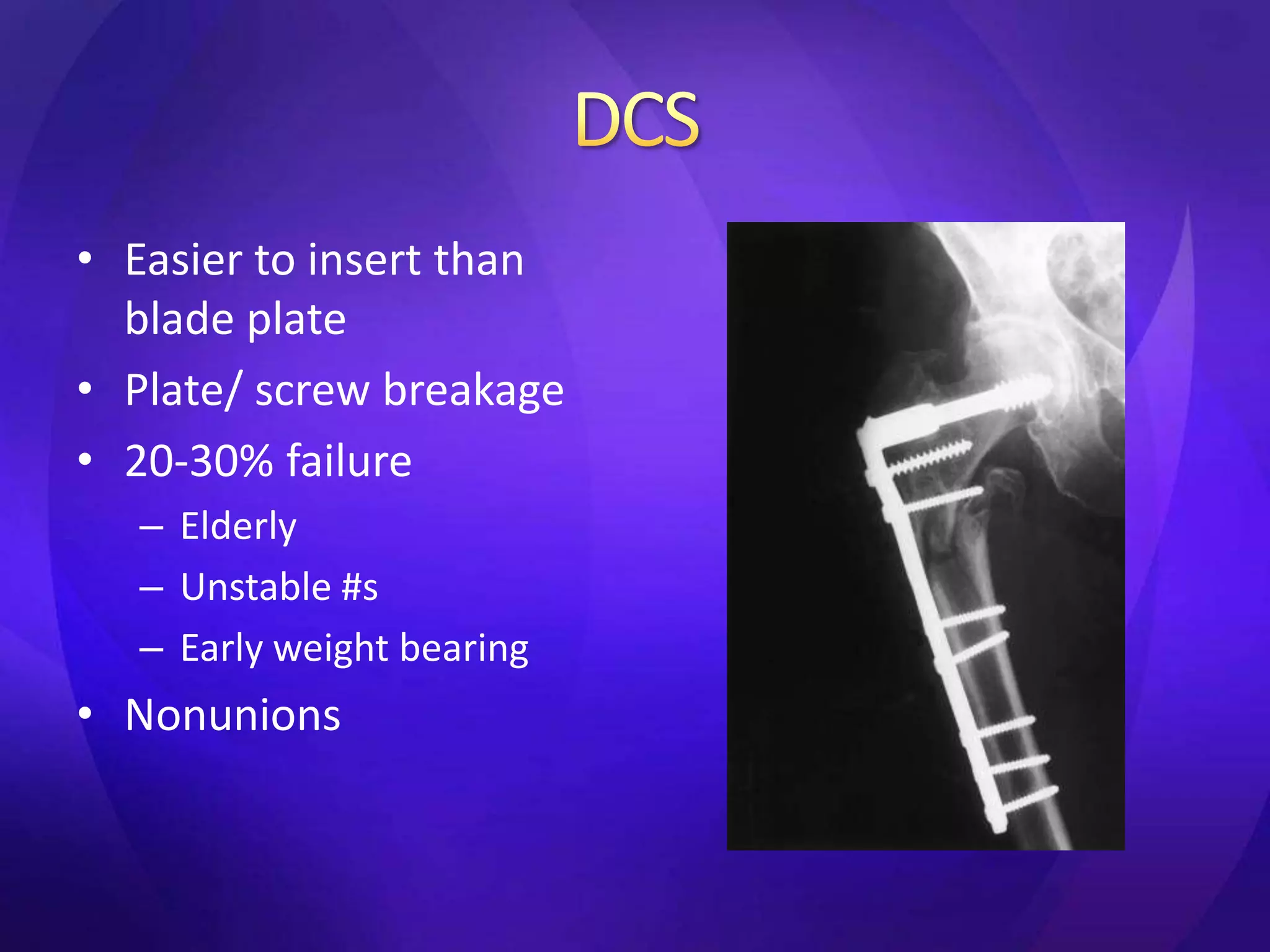
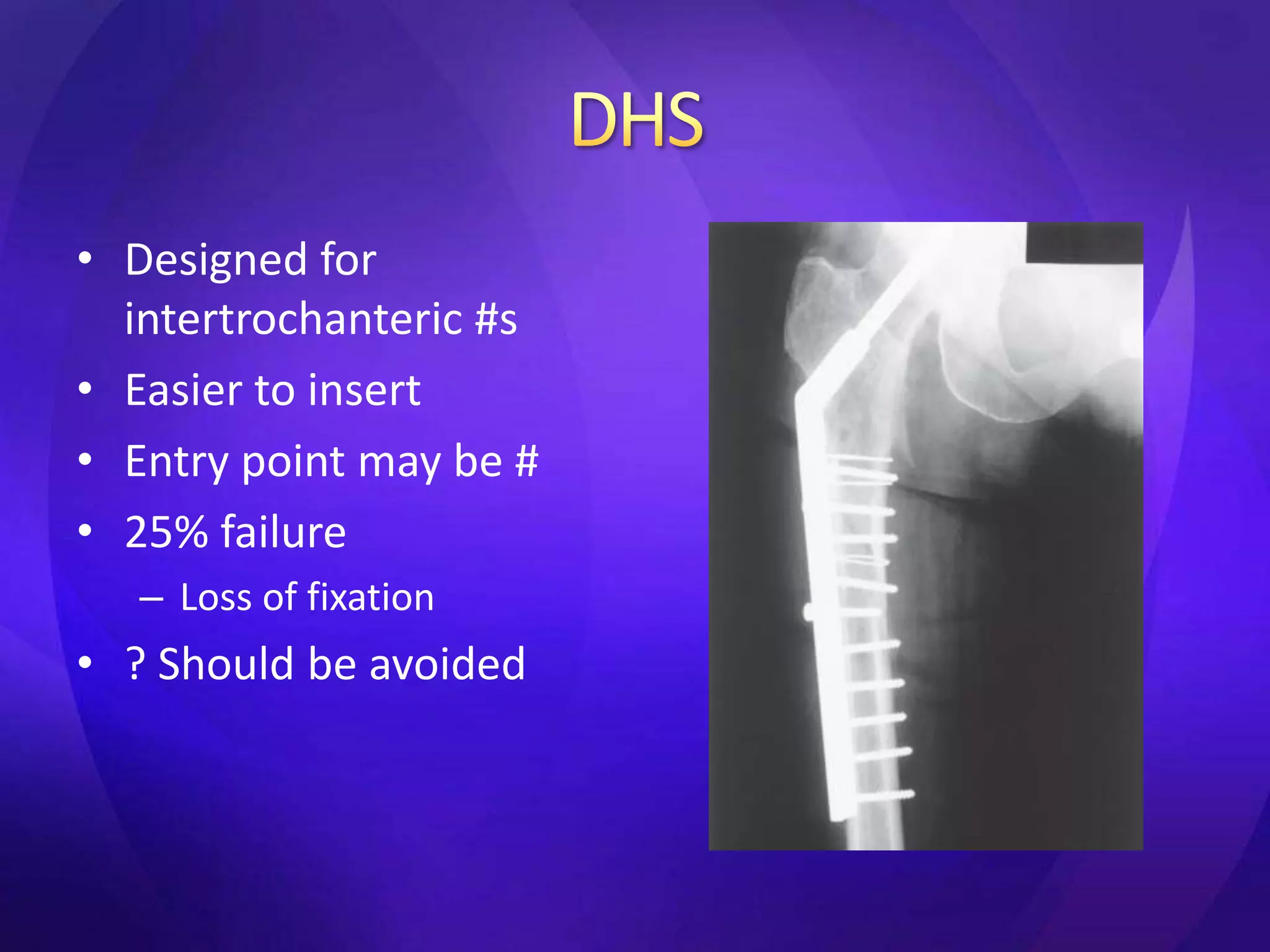
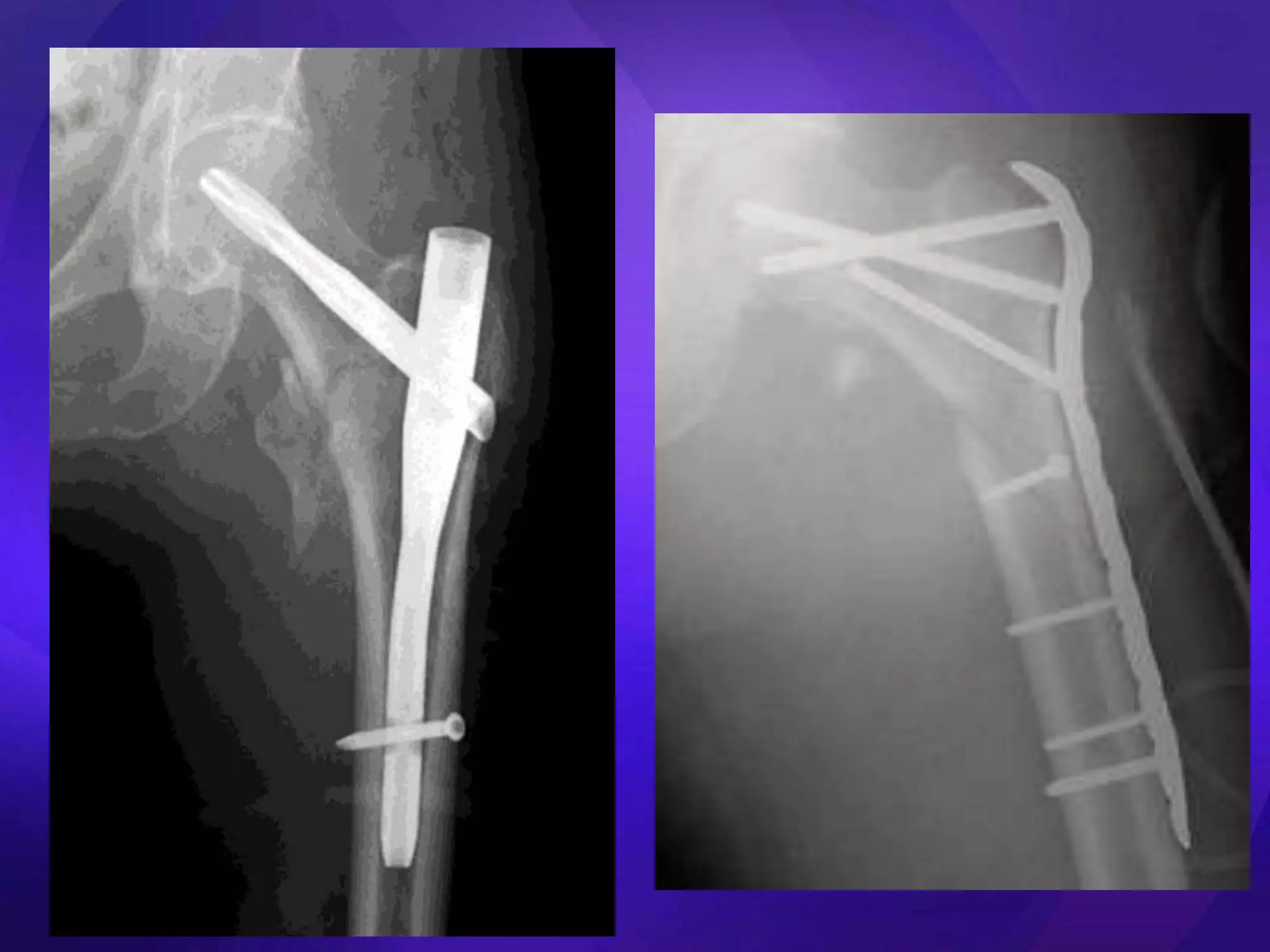
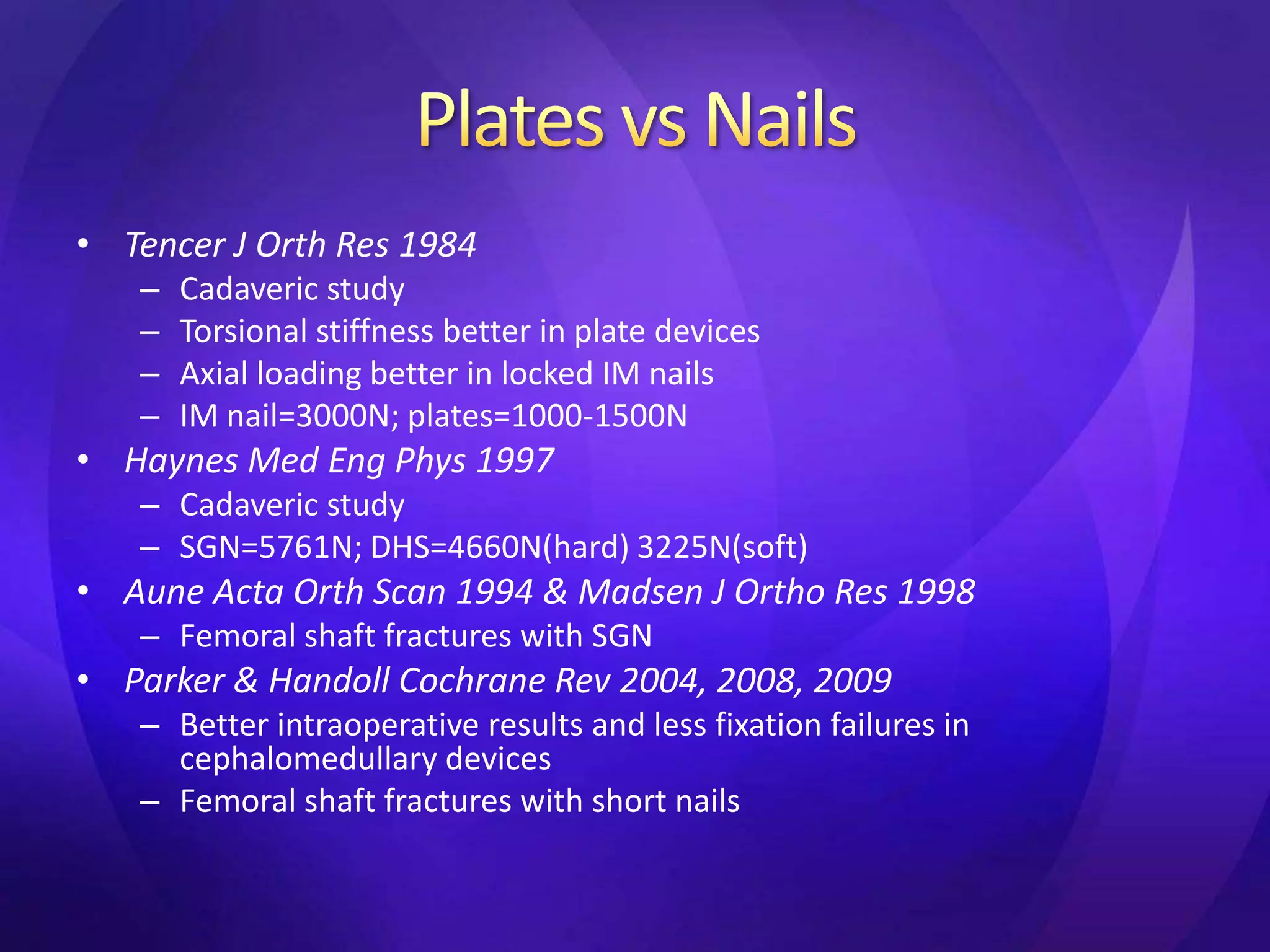
2. It reviews treatment options for subtrochanteric fractures including traction, extramedullary fixation with plates, and intramedullary fixation with nails. Intramedullary nails are preferred as they better resist axial loads and torsion compared to plates.
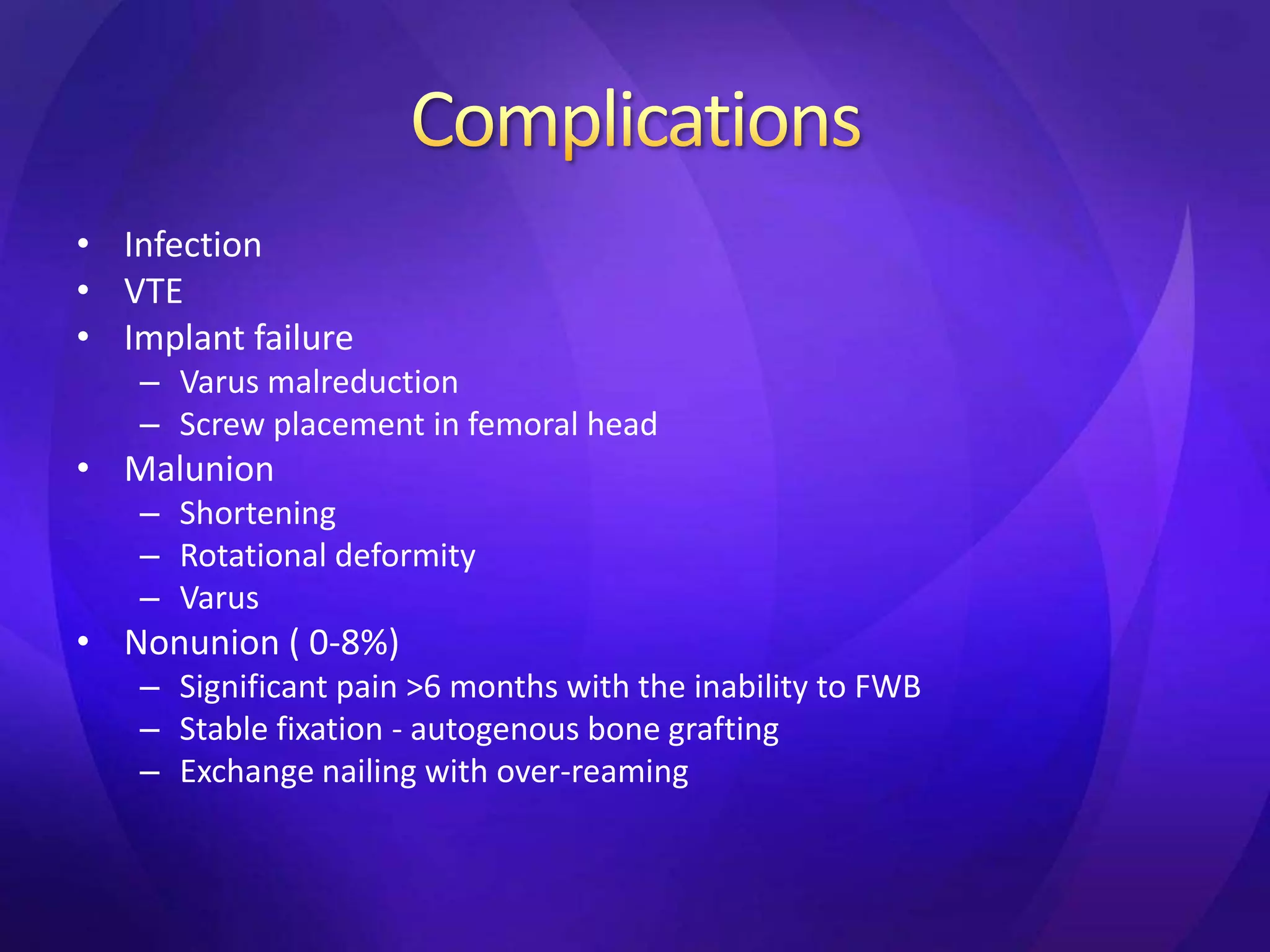
3. Complications of treatment include infection, malunion, nonunion, and implant failure. Proper reduction and fixation are important to