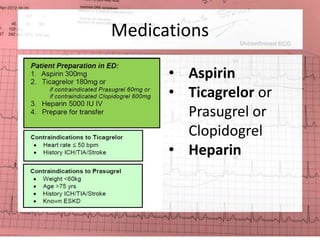
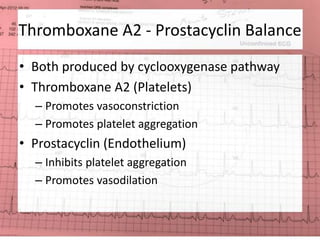
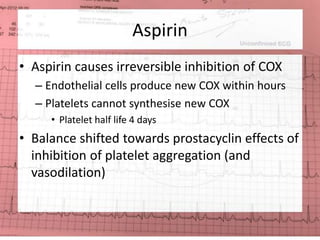
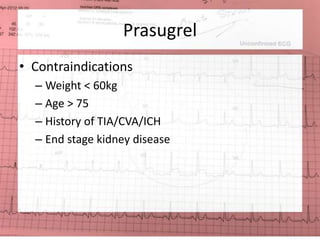
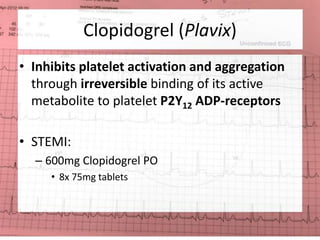
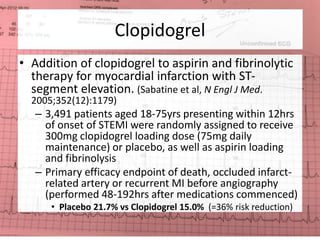
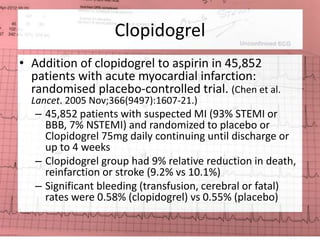
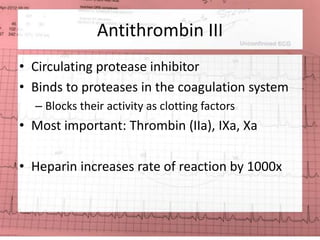
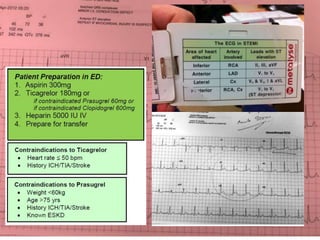
1) Aspirin, P2Y12 inhibitors (ticagrelor, prasugrel, clopidogrel), and heparin are used to treat acute myocardial infarction. Aspirin and P2Y12 inhibitors prevent platelet aggregation while heparin inhibits thrombin.
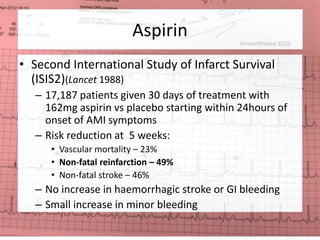
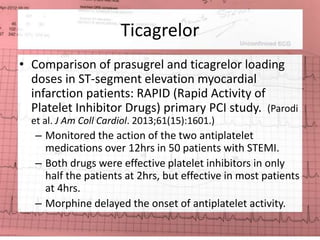
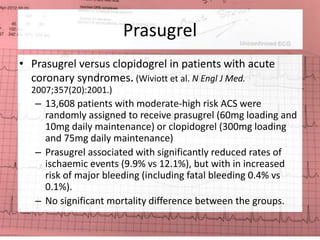
2) Clinical trials have shown that aspirin reduces mortality and reinfarction rates compared to placebo. P2Y12 inhibitors like ticagrelor and prasugrel are more effective than clopidogrel but increase bleeding risk.
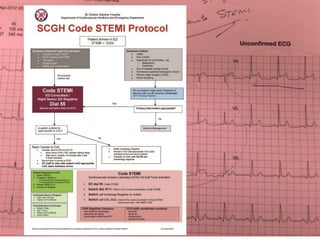
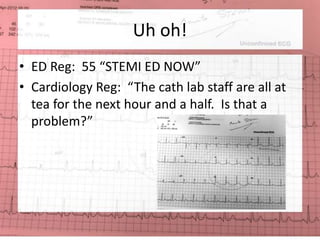
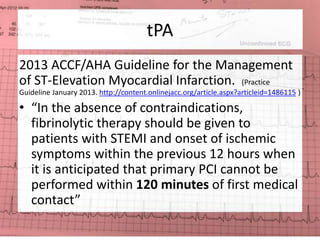
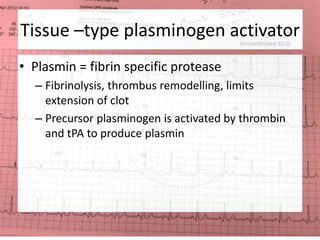
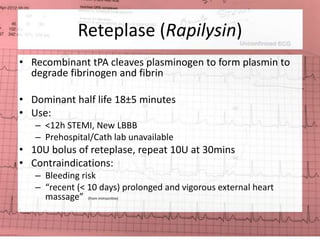
3) Fibrinolytics like tenecteplase can be used when primary PCI is not available within 120 minutes to reperfuse the infarcted area through