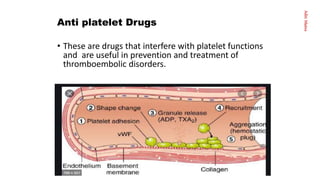
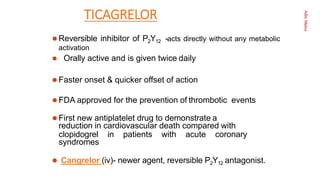
This document provides an overview of hemostasis and antithrombotic drugs. It discusses the four phases of hemostasis - vascular, platelet, coagulation, and fibrinolytic. Antithrombotic drugs include antiplatelet drugs that inhibit platelet activation and aggregation, anticoagulants that inhibit fibrin formation, and fibrinolytic agents that degrade fibrin. The document focuses on antiplatelet drugs, describing their mechanisms of action, types including aspirin, clopidogrel, prasugrel, ticagrelor, and glycoprotein IIb/IIIa antagonists. Their uses, pharmacokinetics, adverse effects, and interactions are summarized.