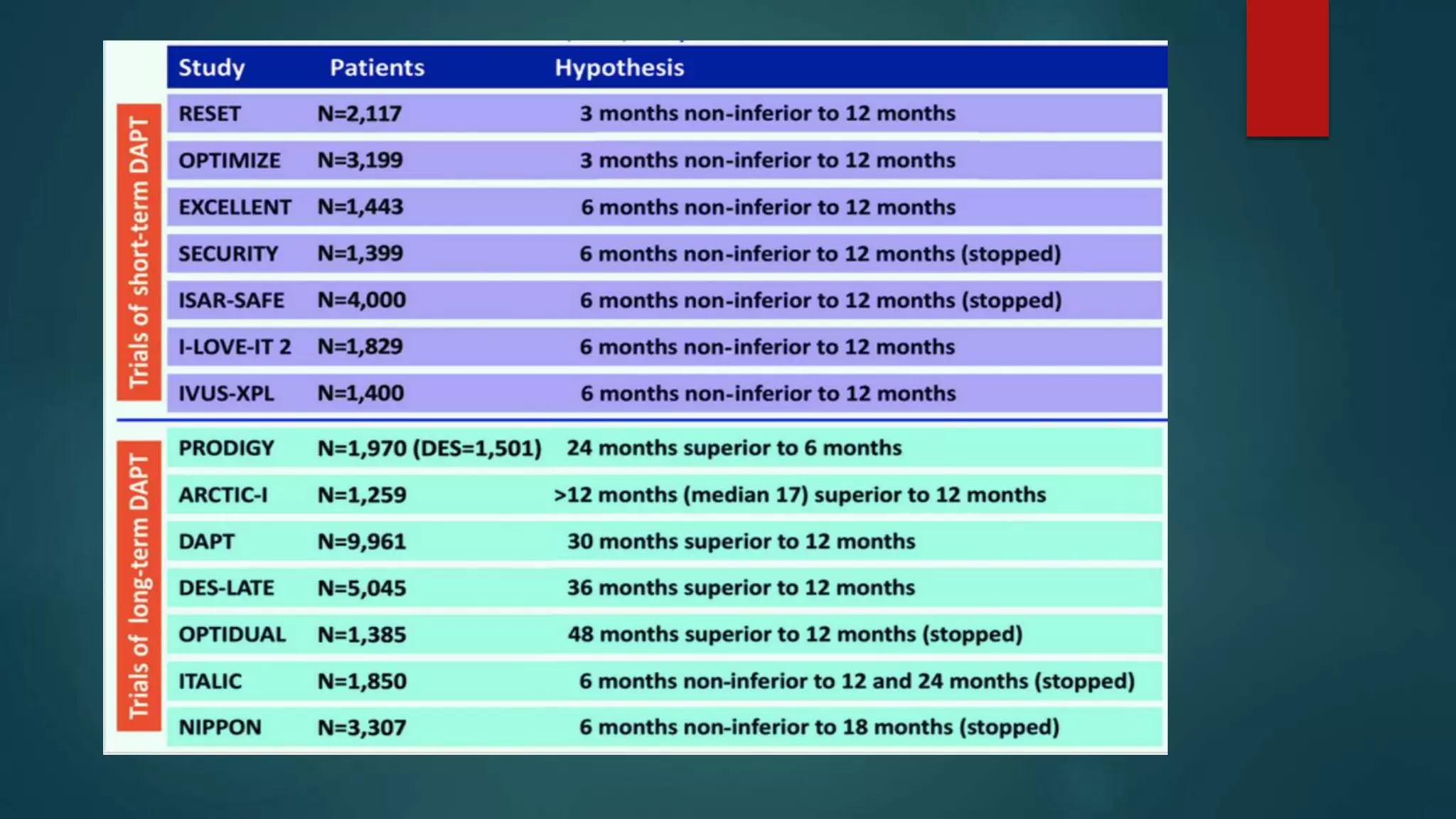
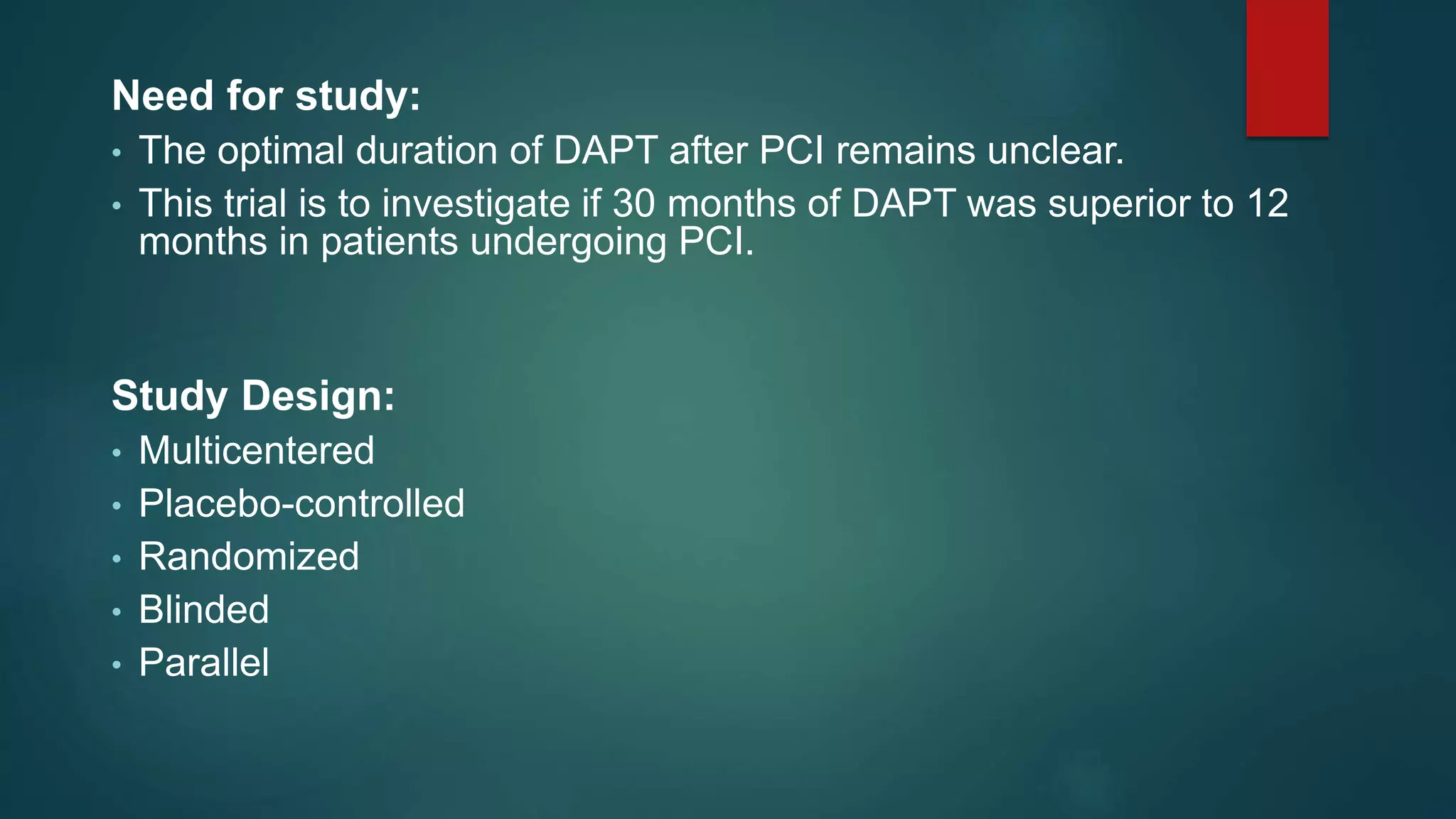
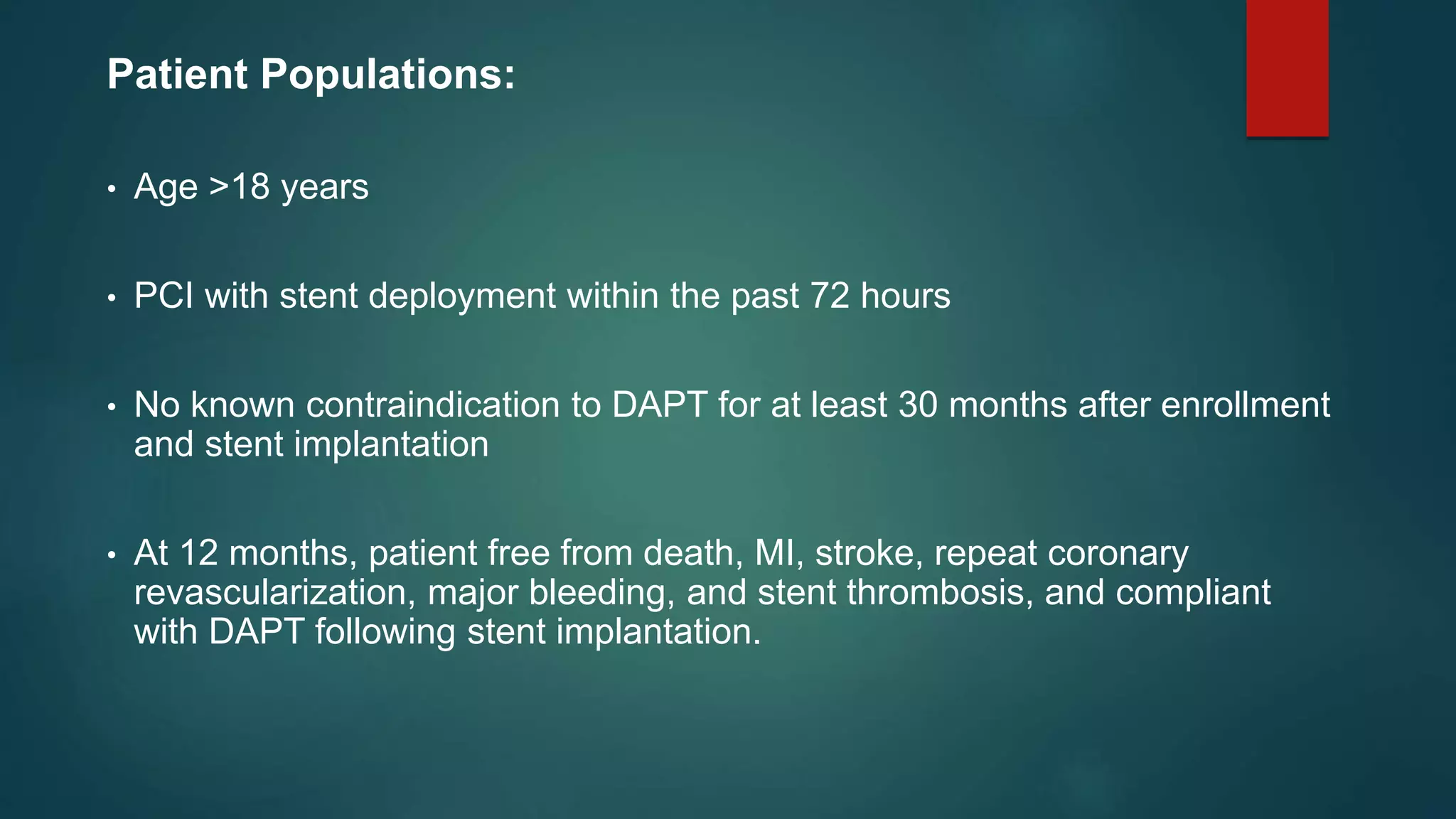
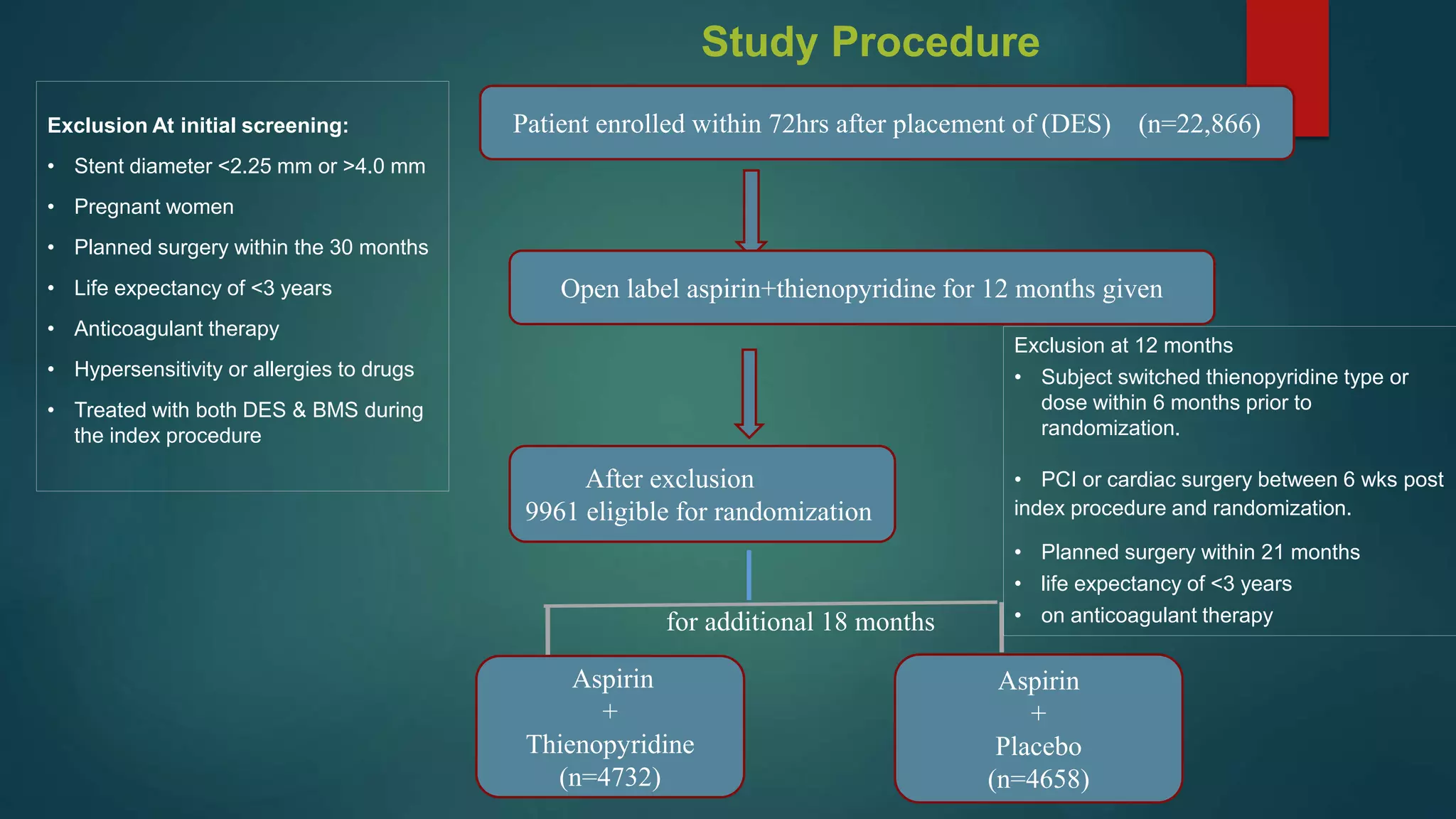
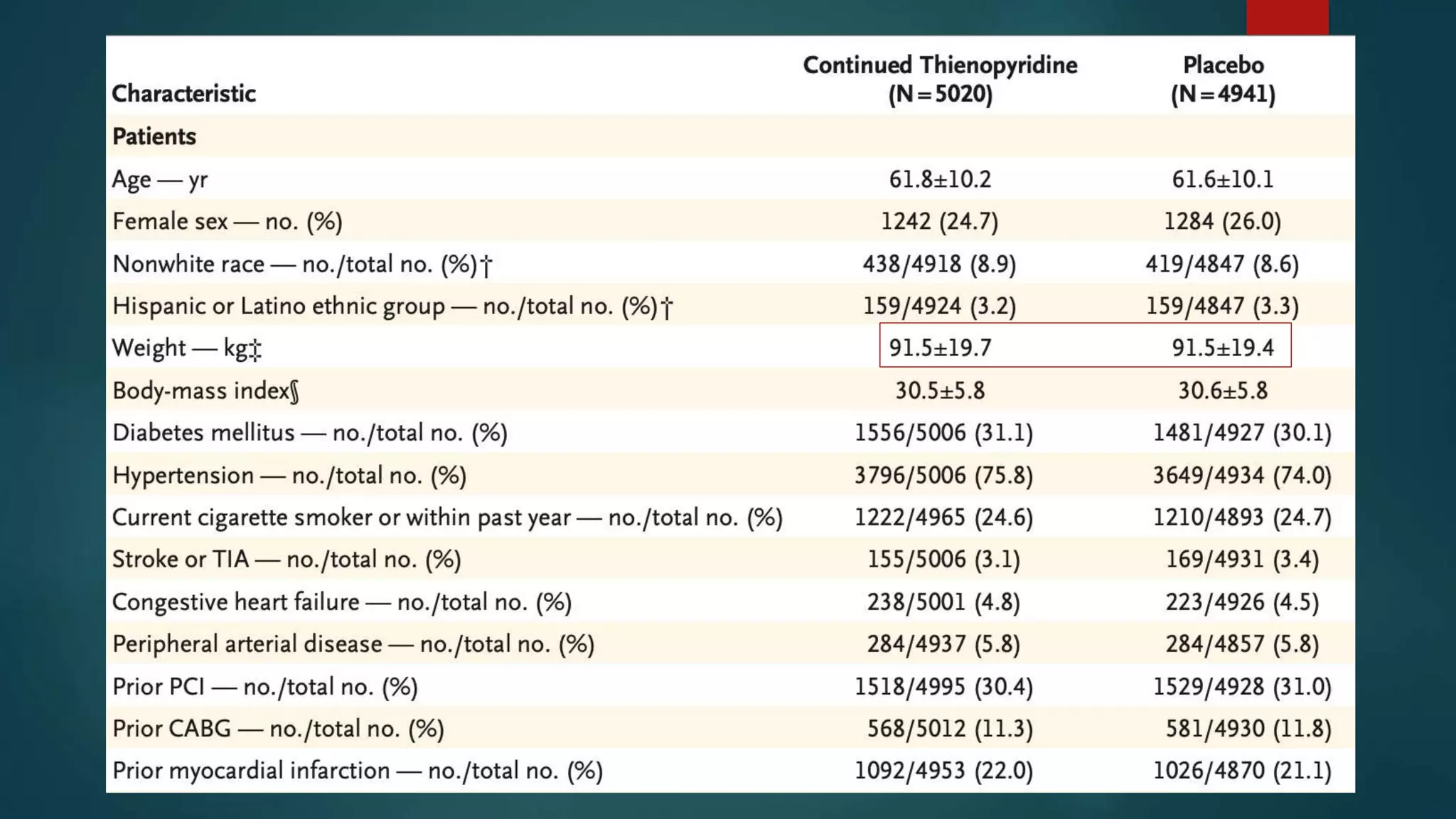
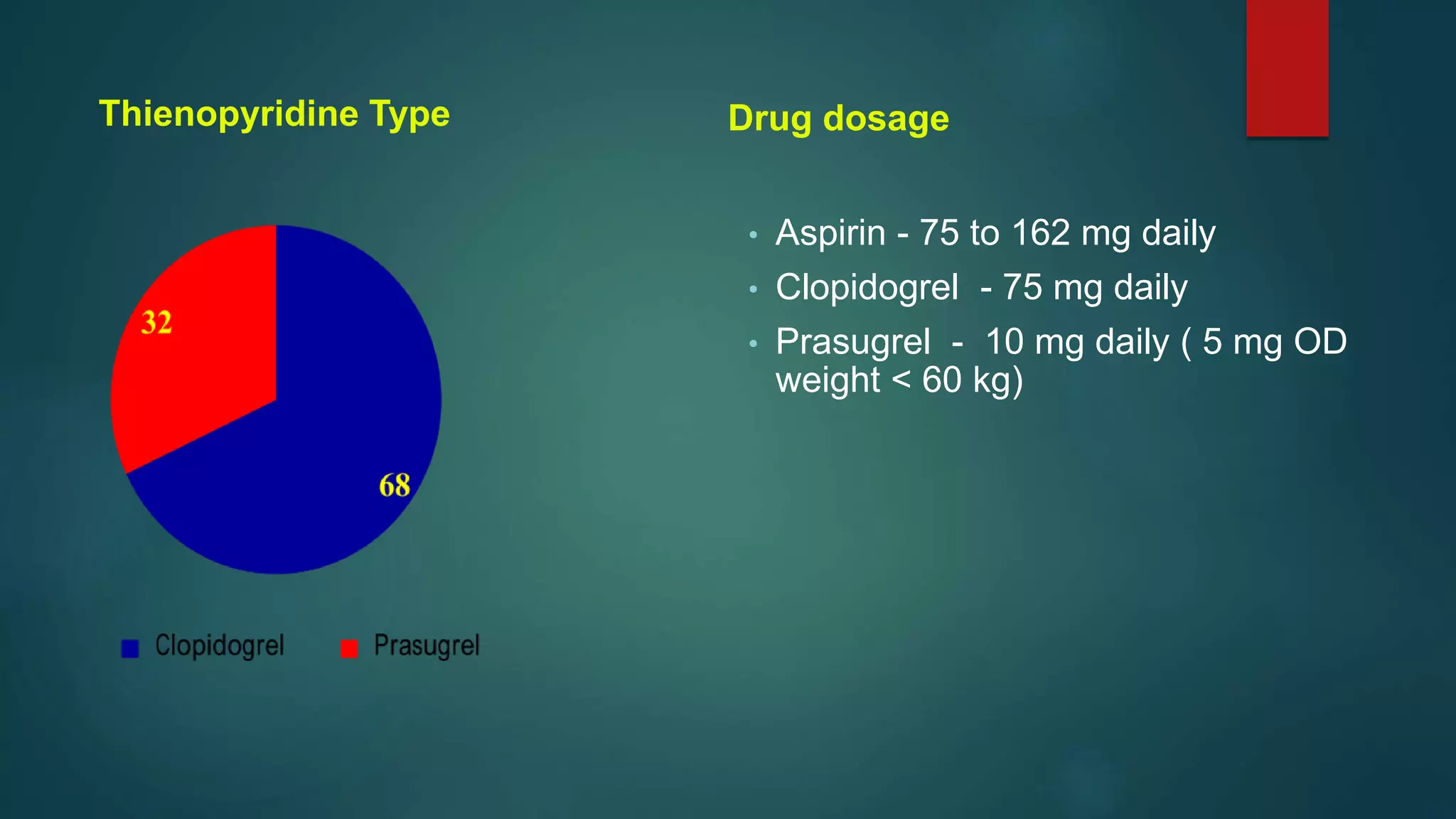
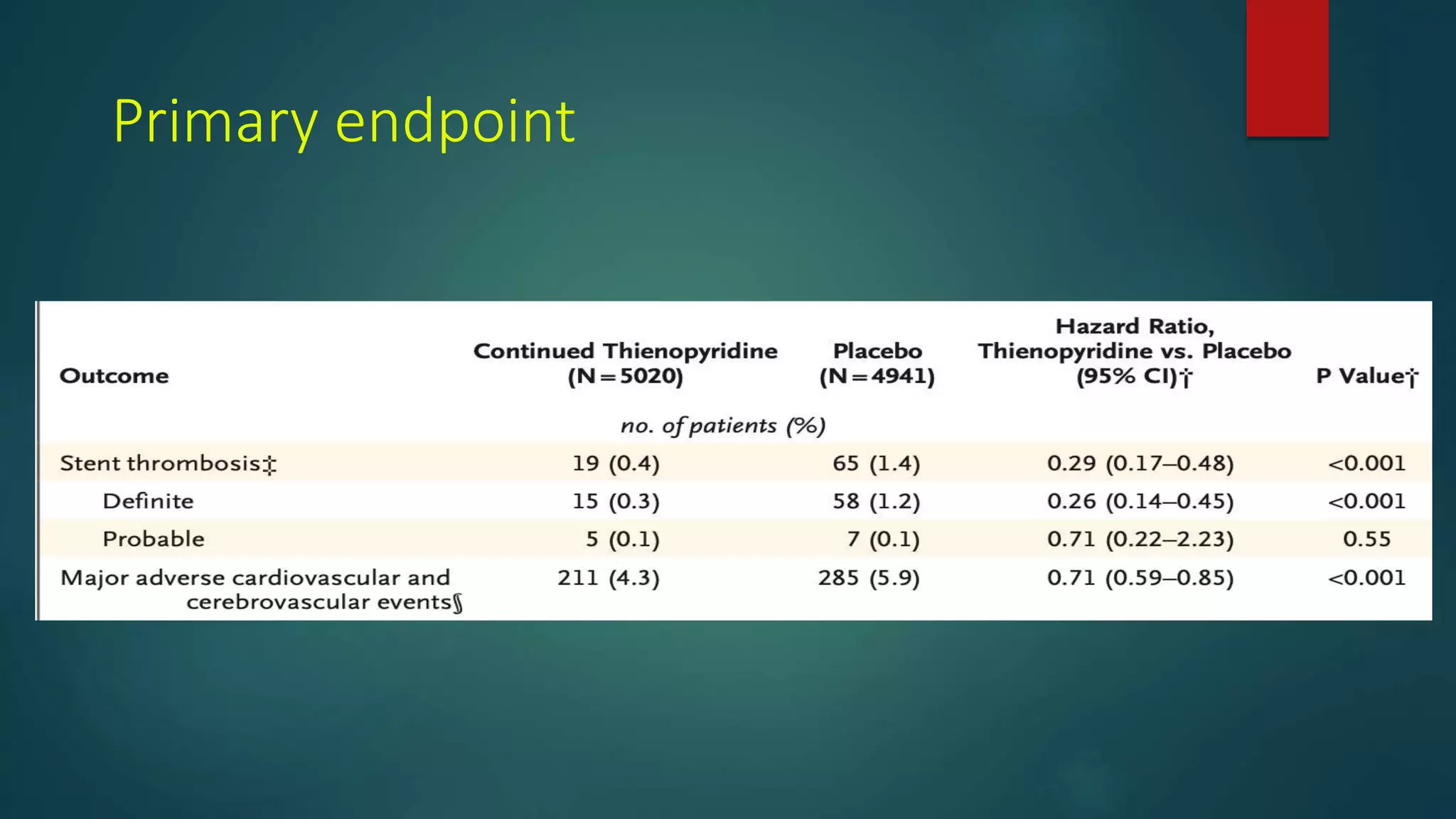
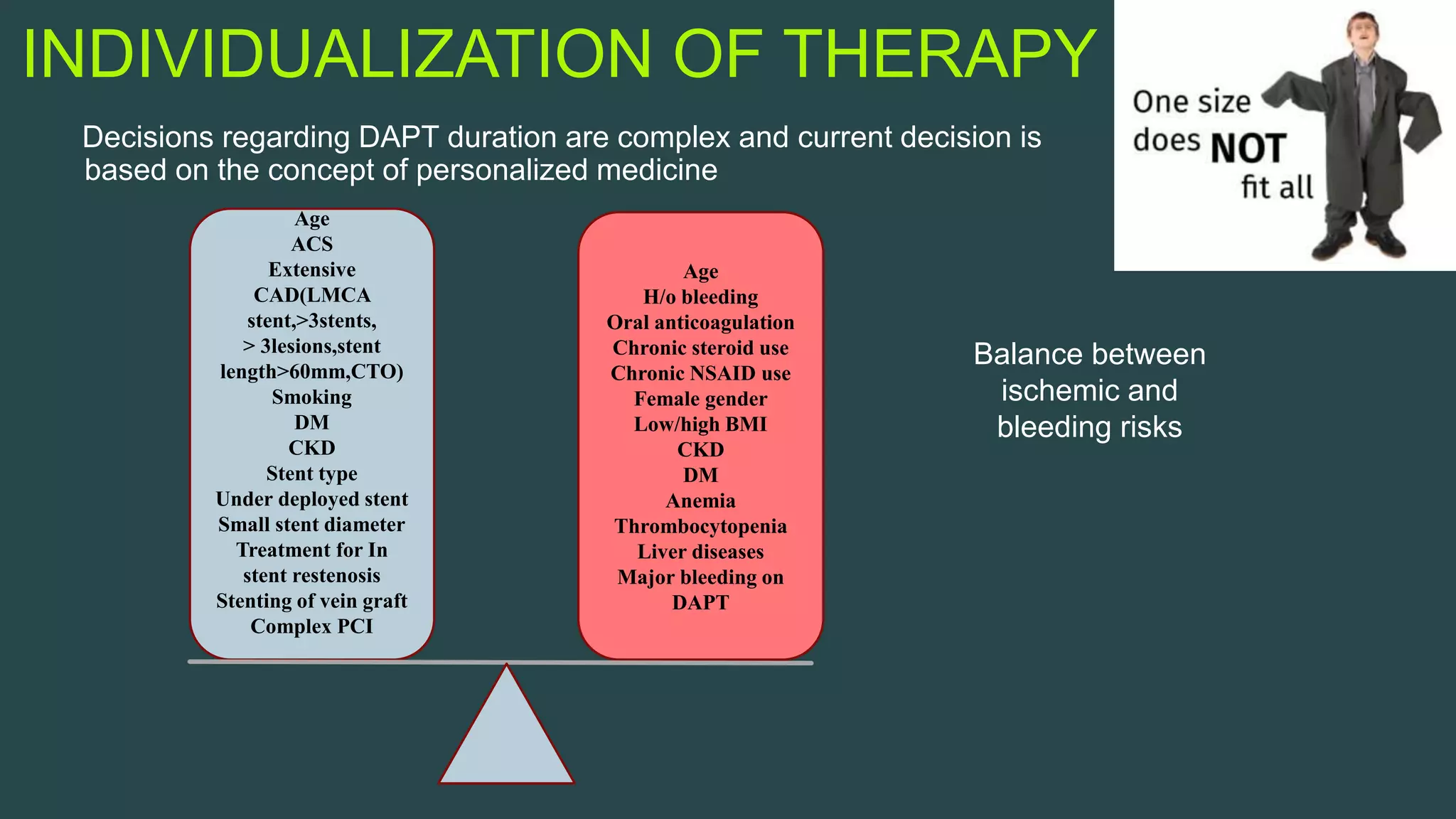
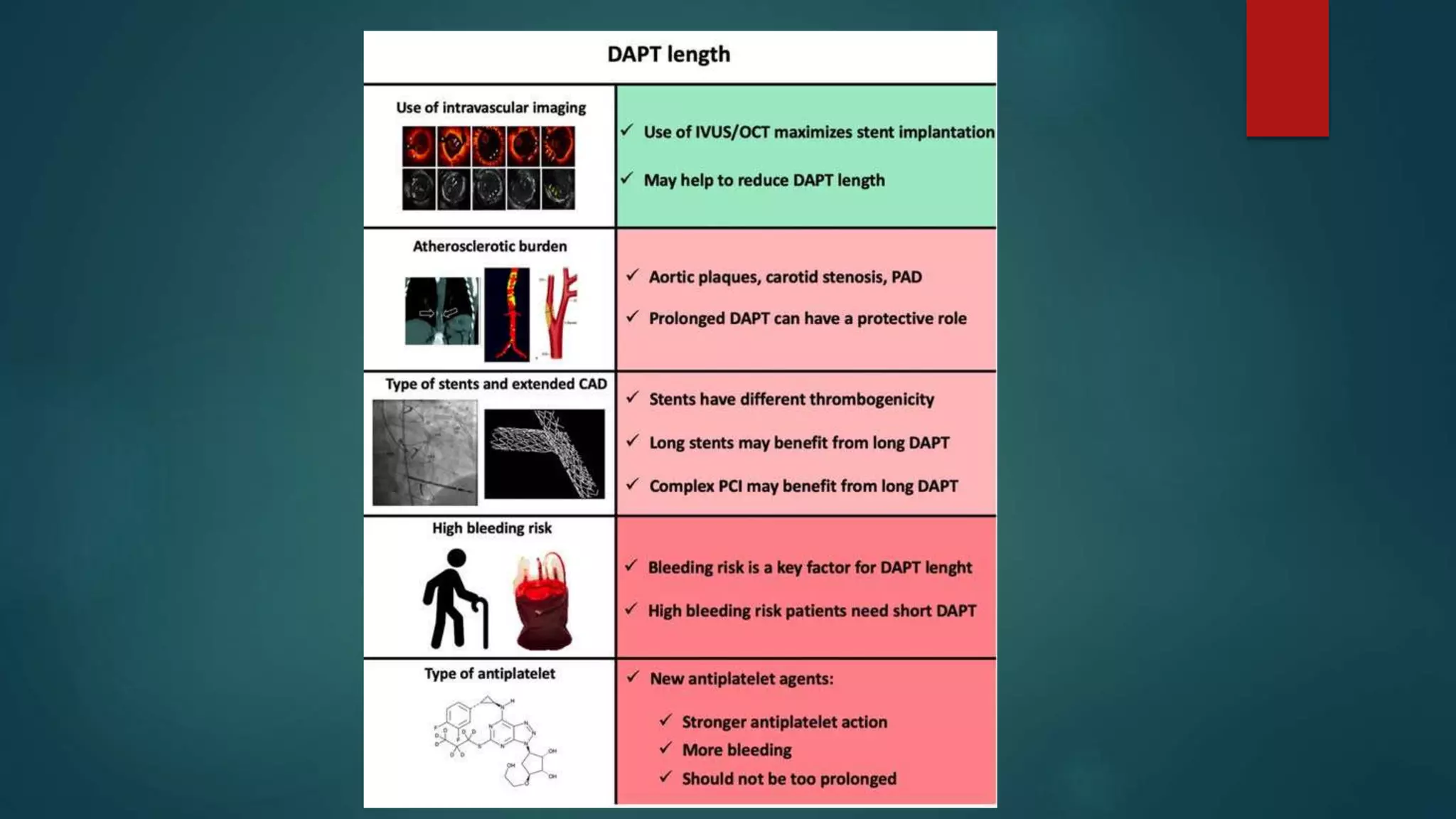
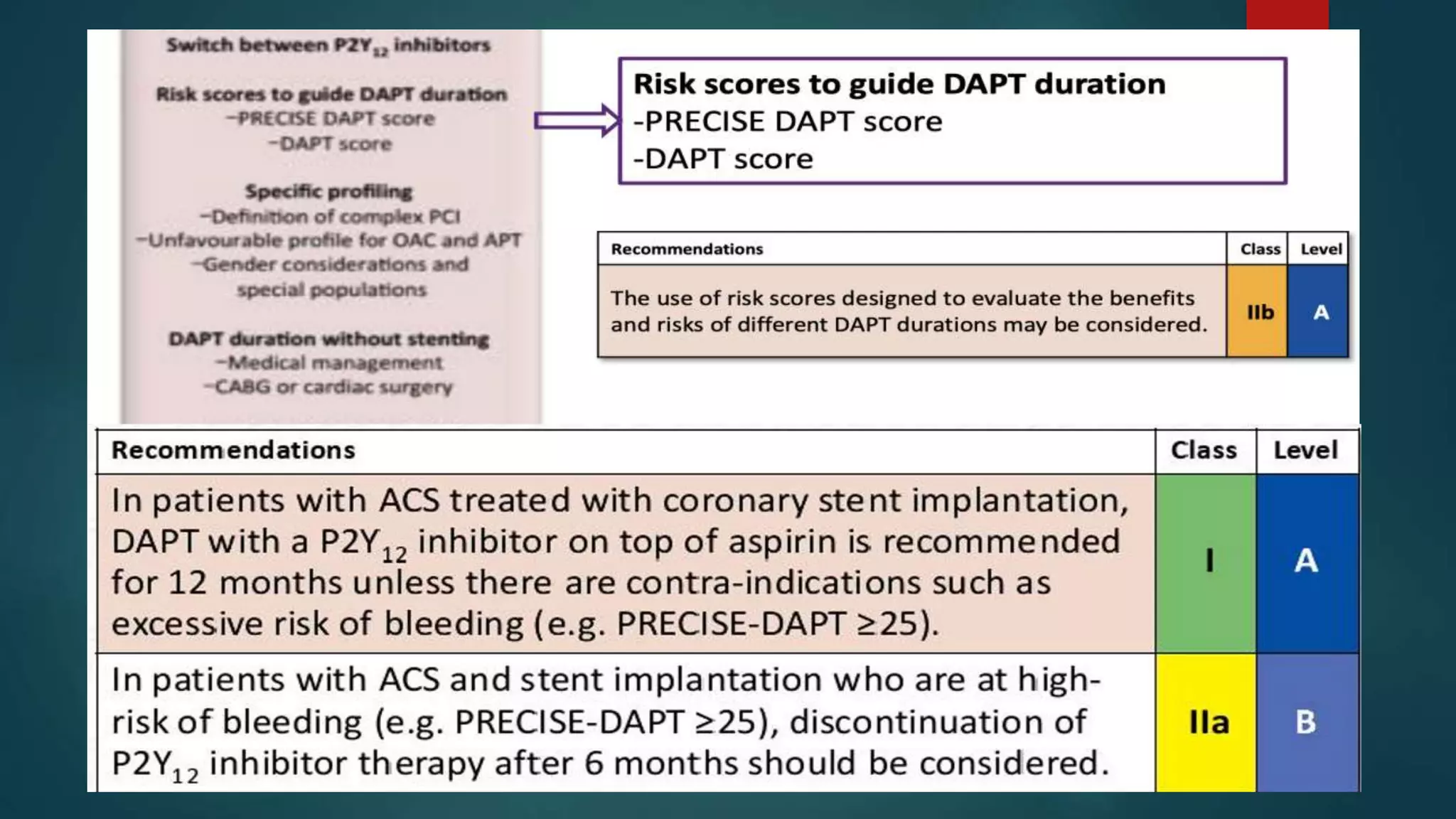
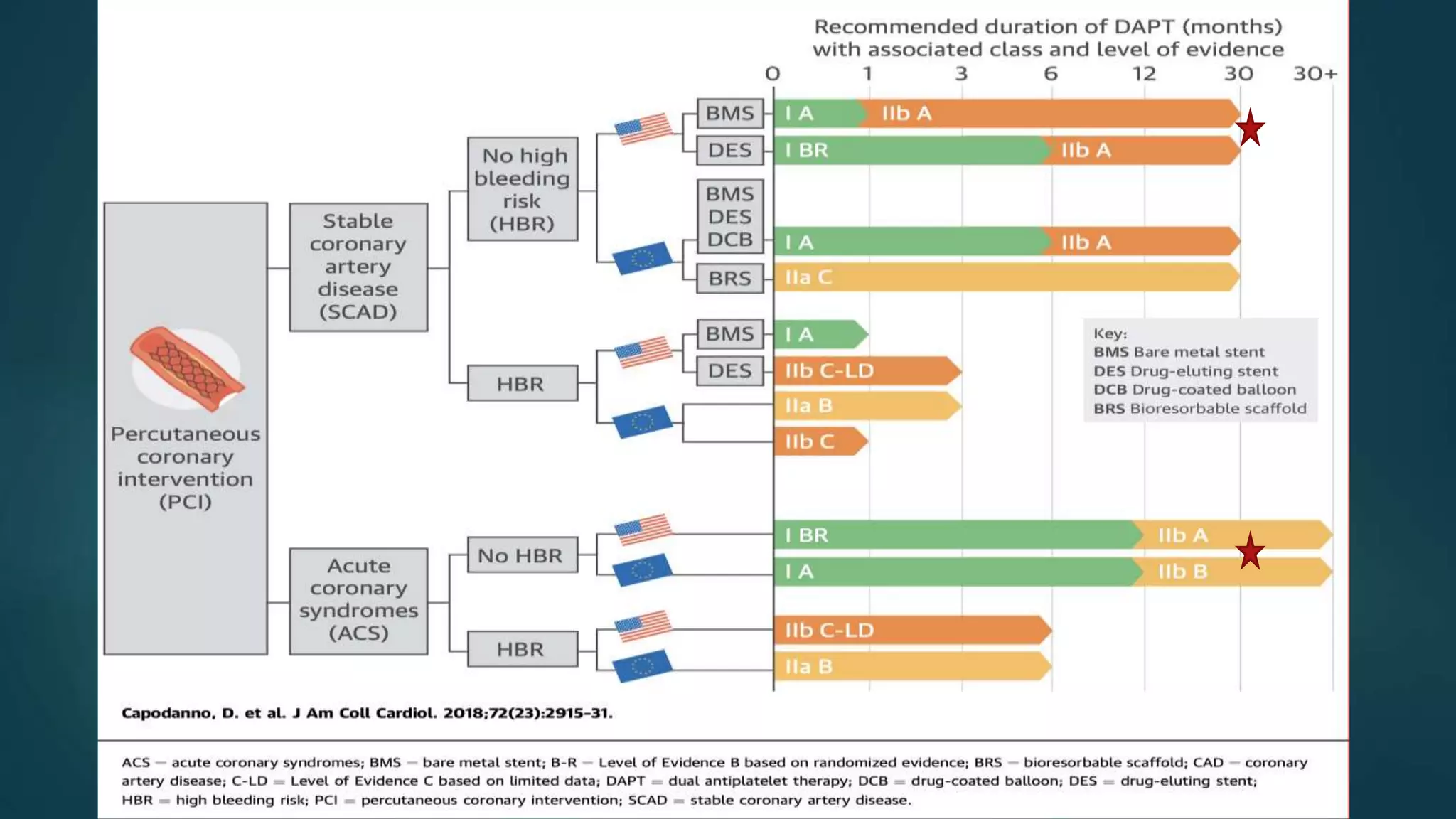
DAPT trial evaluated whether 30 months of dual antiplatelet therapy (DAPT) was superior to 12 months in patients undergoing percutaneous coronary intervention (PCI) with drug-eluting stent placement. The trial found that prolonged DAPT reduced stent thrombosis and major adverse cardiac and cerebrovascular events compared to aspirin alone, but increased bleeding risk. An analysis of the trial developed the DAPT score to predict ischemic and bleeding risks and help determine optimal DAPT duration for individual patients. Newer PRECISE-DAPT and other scores further refine risk stratification to personalize DAPT duration based on balancing ischemic benefit versus bleeding risk.