This document discusses antimalarial drugs. It provides information on:
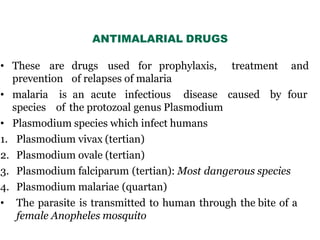
1. Antimalarial drugs are used for prophylaxis, treatment, and prevention of malaria relapses. Malaria is caused by Plasmodium parasites transmitted via mosquito bites.
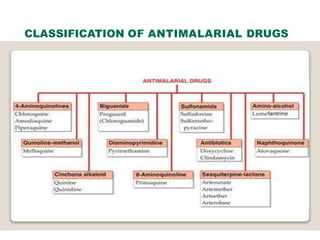
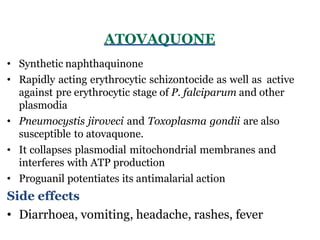
2. Common antimalarial drugs include chloroquine, mefloquine, quinine, primaquine, proguanil, pyrimethamine, and sulfadoxine-pyrimethamine combinations.
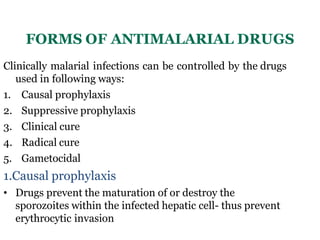
3. These drugs act on different life stages of the malaria parasite and are used for prevention, treatment, radical cure, and blocking transmission to mosquitoes. Adverse effects and mechanisms of action are described for major antimal