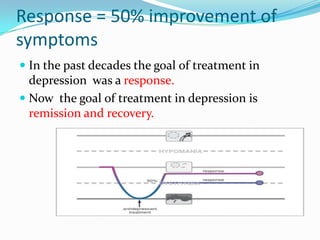
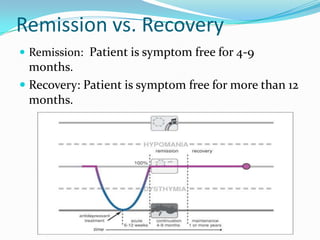
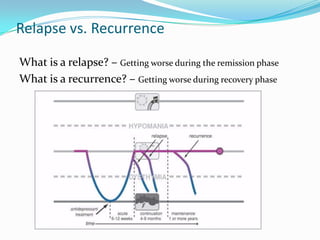
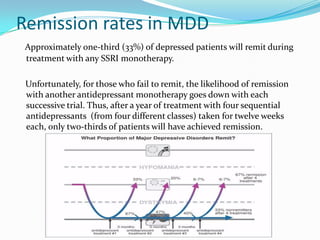
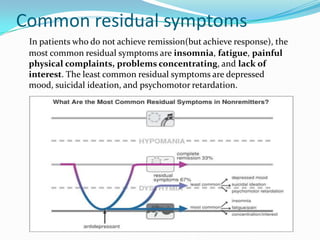
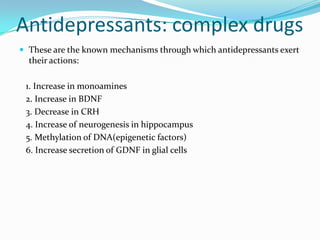
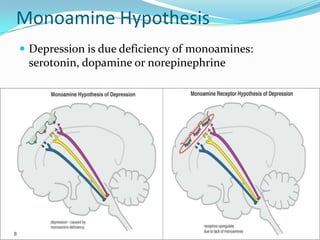
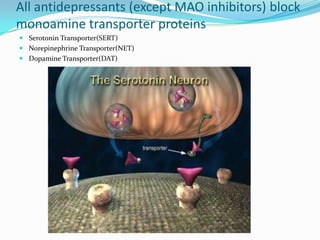
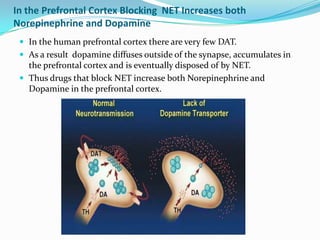
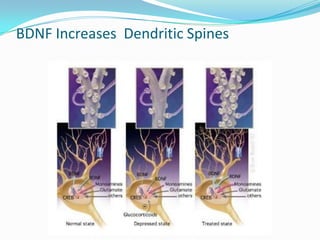
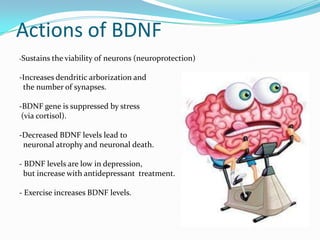
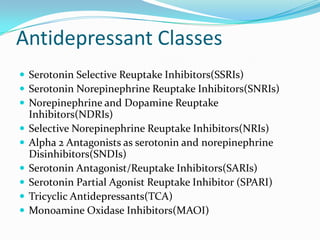
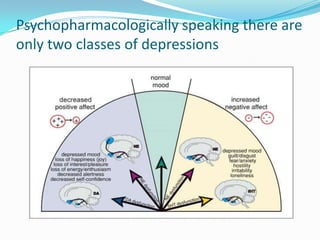
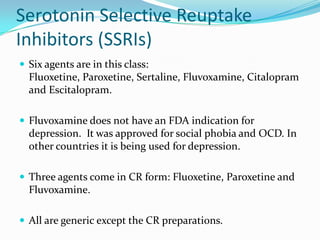
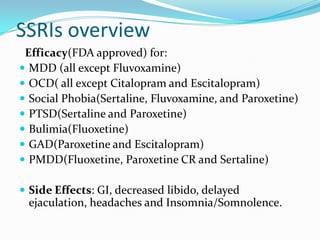
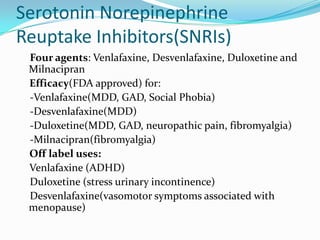
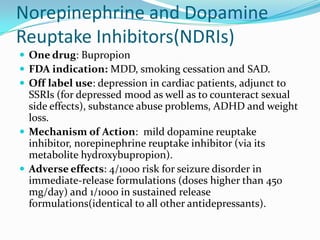
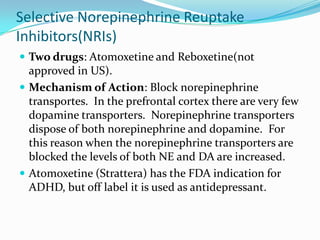
Antidepressants work through multiple mechanisms including increasing monoamines like serotonin, norepinephrine, and dopamine; increasing brain-derived neurotrophic factor (BDNF); and decreasing corticotropin-releasing hormone (CRH). The main classes of antidepressants are SSRIs, SNRIs, NDRIs, NRIs, SARIs, SPARIs, TCAs, and MAOIs. Treatment goals have shifted from response to remission and recovery, though residual symptoms often persist even with response.