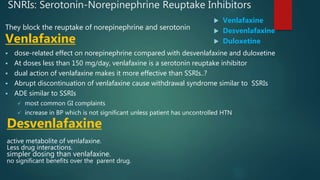
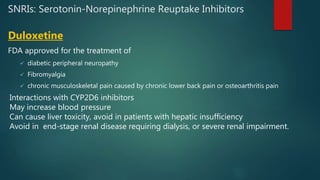
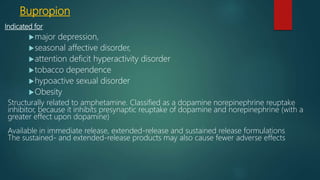
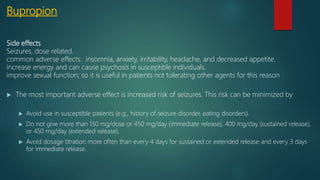
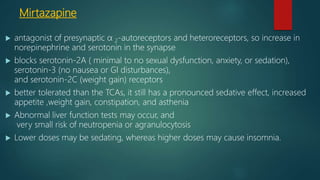
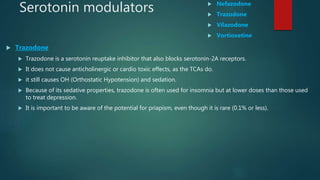
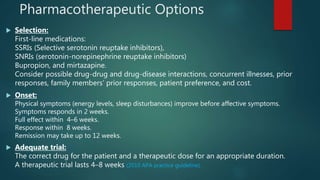
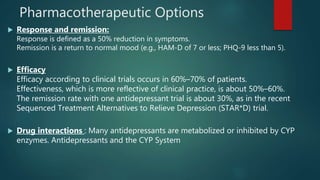
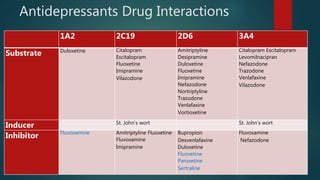
The document discusses updates on antidepressant medications. It covers various antidepressant classes including SSRIs, SNRIs, atypical antidepressants, TCAs, and MAOIs. It describes their mechanisms of action, dosing, efficacy, adverse effects, drug interactions and treatment of treatment-resistant depression. Key trials like STAR*D are also summarized.


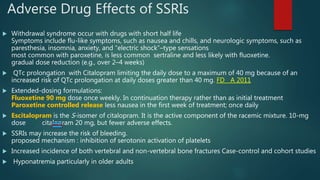
![SSRIs Induced sexual dysfunction
incidence 15% to 80%
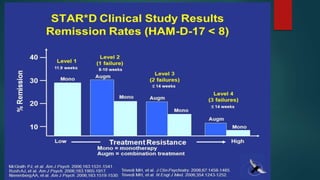
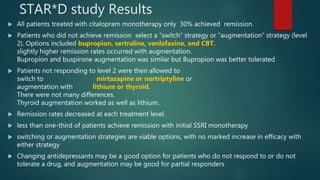
A 14-week, prospective observational study (Sequenced Treatment Alternatives to Relieve Depression [STAR*D]) of 1473
patients treated with citalopram found that
•Decreased libido occurred in 54 percent
•Difficulty achieving orgasm occurred in 36 percent
•Among the 574 males, erectile dysfunction occurred in 37 percent
Treatment options for patients who respond to SSRIs but suffer sexual dysfunction include :
1. Waiting for spontaneous remission of sexual impairment and decreasing the dose
2. Switching to a non-SSRI antidepressant or a different SSRI Bupropion
A network meta-analysis of 37 randomized trials (n >14,000 depressed patients) found that the incidence of sexual
dysfunction was less with bupropion than escitalopram, paroxetine, or sertraline
Sexual dysfunction that emerges during treatment with SSRIs may persist despite switching to bupropion. For these
patients, we suggest discontinuing bupropion and switching to Mirtazapine
meta-analysis of four randomized trials (n = 907 patients with major depression) that compared mirtazapine with
SSRIs (fluoxetine, paroxetine, or sertraline), and found that sexual dysfunction was less likely with mirtazapine (odds
ratio 0.3, 95% CI 0.1-0.7)
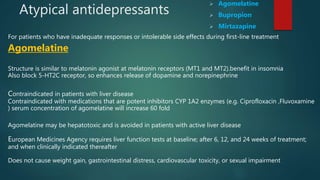
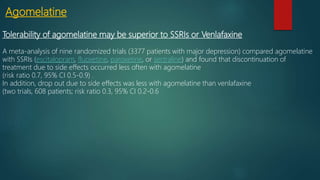
Other alternatives to mirtazapine include Agomelatine, Nefazodone
3. Augment with a second drug phosphodiesterase-5 inhibitors or bupropion
For men with erectile dysfunction, treatment with a phosphodiesterase-5 inhibitor, rather than bupropion .
For women with sexual dysfunction, add-on bupropion at higher doses rather than a phosphodiesterase-5 inhibitor](https://image.slidesharecdn.com/updatesonantidepressantmedications-191220105119/85/Updates-on-antidepressant-medications-12-320.jpg)