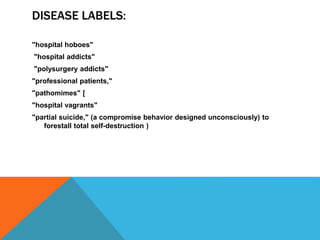
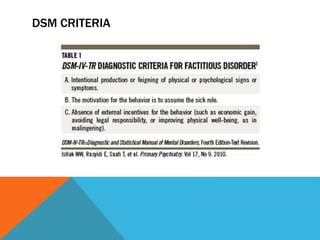
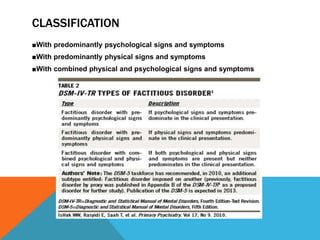
This document provides an overview of factitious disorder, including its history, definitions, subtypes, proposed causes and risk factors, demographics of those affected, treatment approaches, and diagnostic testing considerations. It describes how factitious disorder was first documented by Galen and later studied by Richard Asher in 1951. Key points covered include the deliberate falsification of physical or psychological symptoms for the purpose of assuming the sick role, potential psychodynamic drivers like seeking attention or nurturing, and challenges in treating those diagnosed due to lack of follow through.