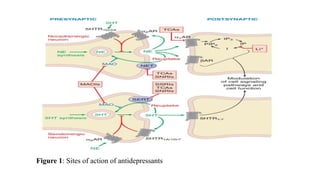
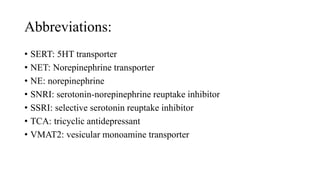
This document discusses depression and various antidepressant drugs. It defines depression and its types. It explains the mechanisms of depression involving neurotransmitters like serotonin, dopamine and norepinephrine. It then describes various classes of antidepressant drugs like SSRIs, SNRIs, MAOIs, TCAs and atypical antidepressants. It explains the mechanisms of action of these drug classes in increasing neurotransmitter levels in the brain. SSRIs and SNRIs inhibit reuptake of serotonin and norepinephrine. MAOIs inhibit the enzyme monoamine oxidase. TCAs inhibit reuptake of serotonin, norepinephrine and dopamine. The document provides examples of drugs in each class.