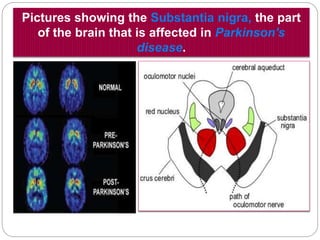
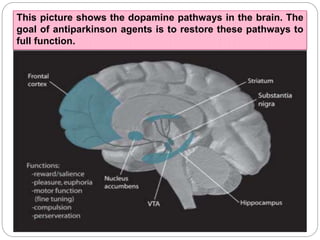
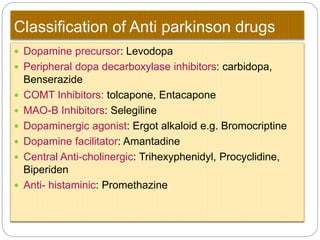
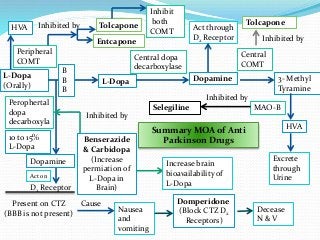
Parkinson's disease is a progressive nervous system disorder that causes a loss of dopamine-producing brain cells, leading to motor symptoms like tremors and rigidity. It occurs due to degeneration of the substantia nigra, decreasing dopamine levels in the basal ganglia. The document discusses the causes, symptoms, diagnosis, treatment and management of Parkinson's disease with a focus on increasing dopamine levels through drugs like L-DOPA, COMT inhibitors, and dopamine receptor agonists.