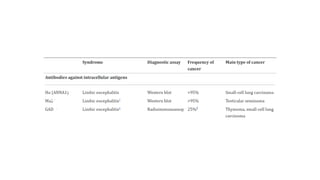
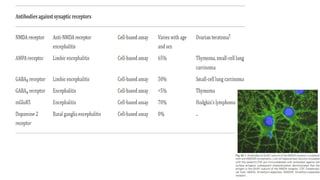
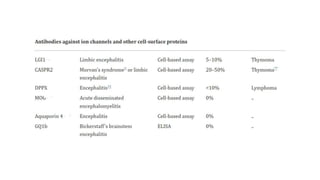
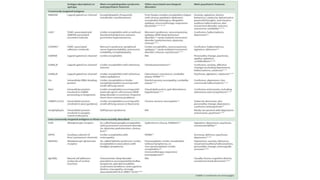
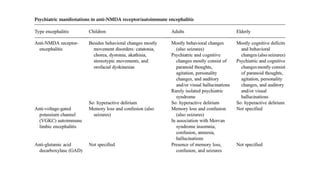
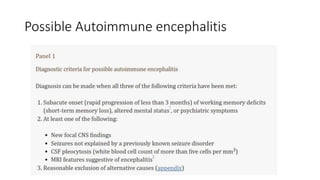
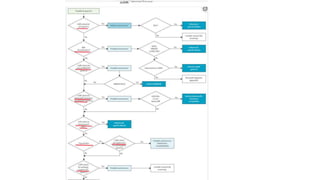
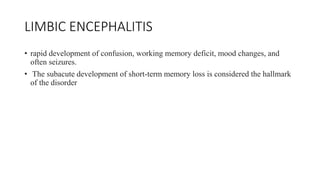
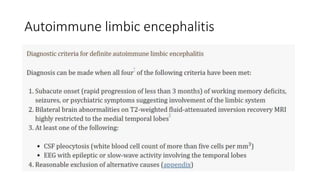
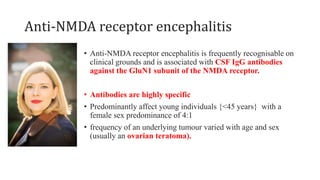
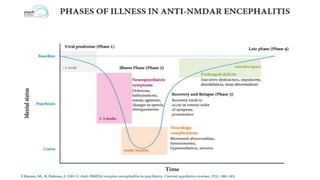
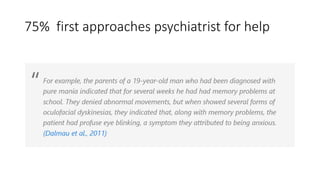
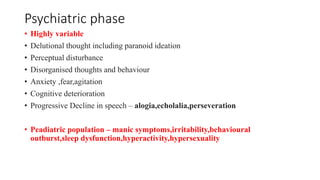
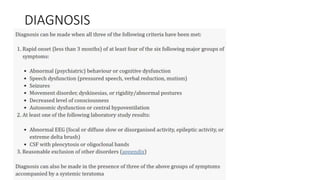
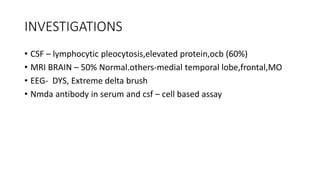
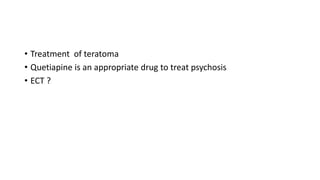
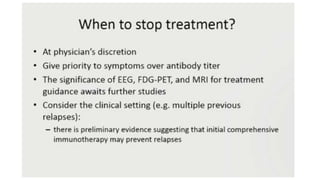
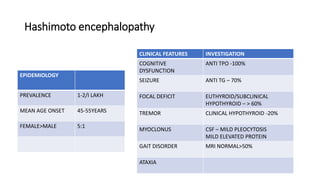
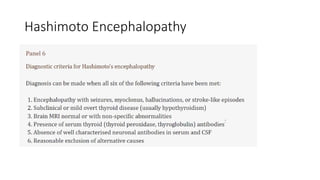
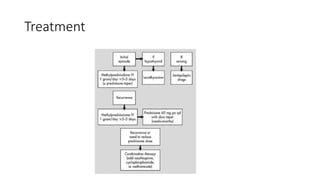
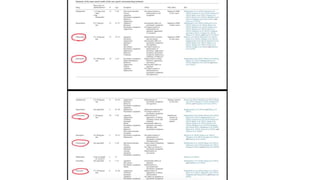
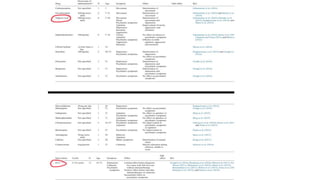
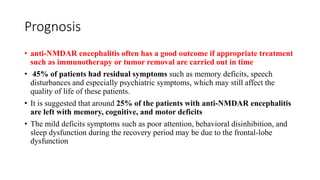
The document discusses autoimmune encephalitis, outlining its types, psychiatric manifestations, diagnostic indicators, and treatment options. It highlights the role of specific antibodies, particularly in conditions like anti-NMDA receptor encephalitis, which primarily affects young females and can present with a variety of psychiatric symptoms. Prognosis is generally positive with appropriate treatment, though some patients may experience residual cognitive and psychiatric difficulties post-recovery.