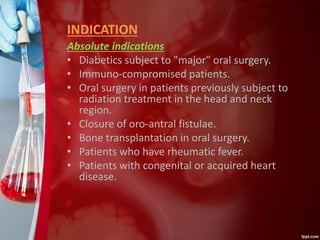
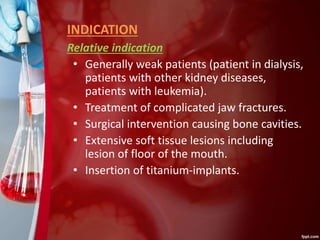
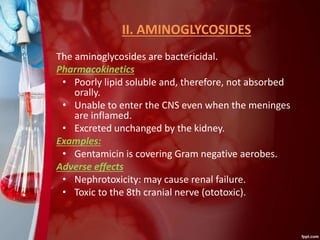
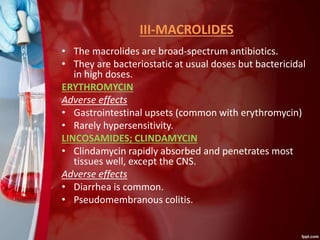
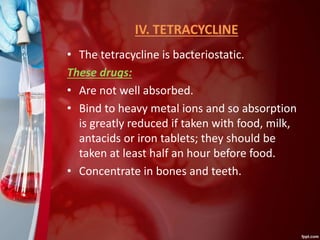
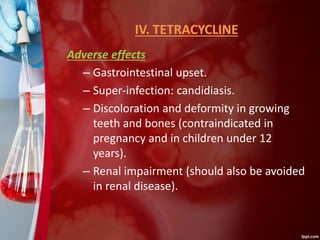
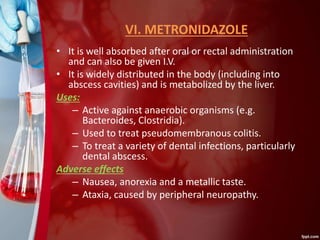
This document discusses different types of antibiotics, including their definitions, indications, mechanisms of action, and resistance. It describes several classes of antibiotics: beta-lactams like penicillin and cephalosporin which inhibit bacterial cell wall synthesis; aminoglycosides which have nephrotoxicity risks; macrolides like erythromycin which are bacteriostatic; tetracyclines which can discolor teeth and bones; and metronidazole which is effective against anaerobic bacteria. Each antibiotic class has different spectrums of activity, mechanisms of action, pharmacokinetics, uses, and potential adverse effects. Precise indications and risks are outlined to help guide appropriate clinical antibiotic selection and