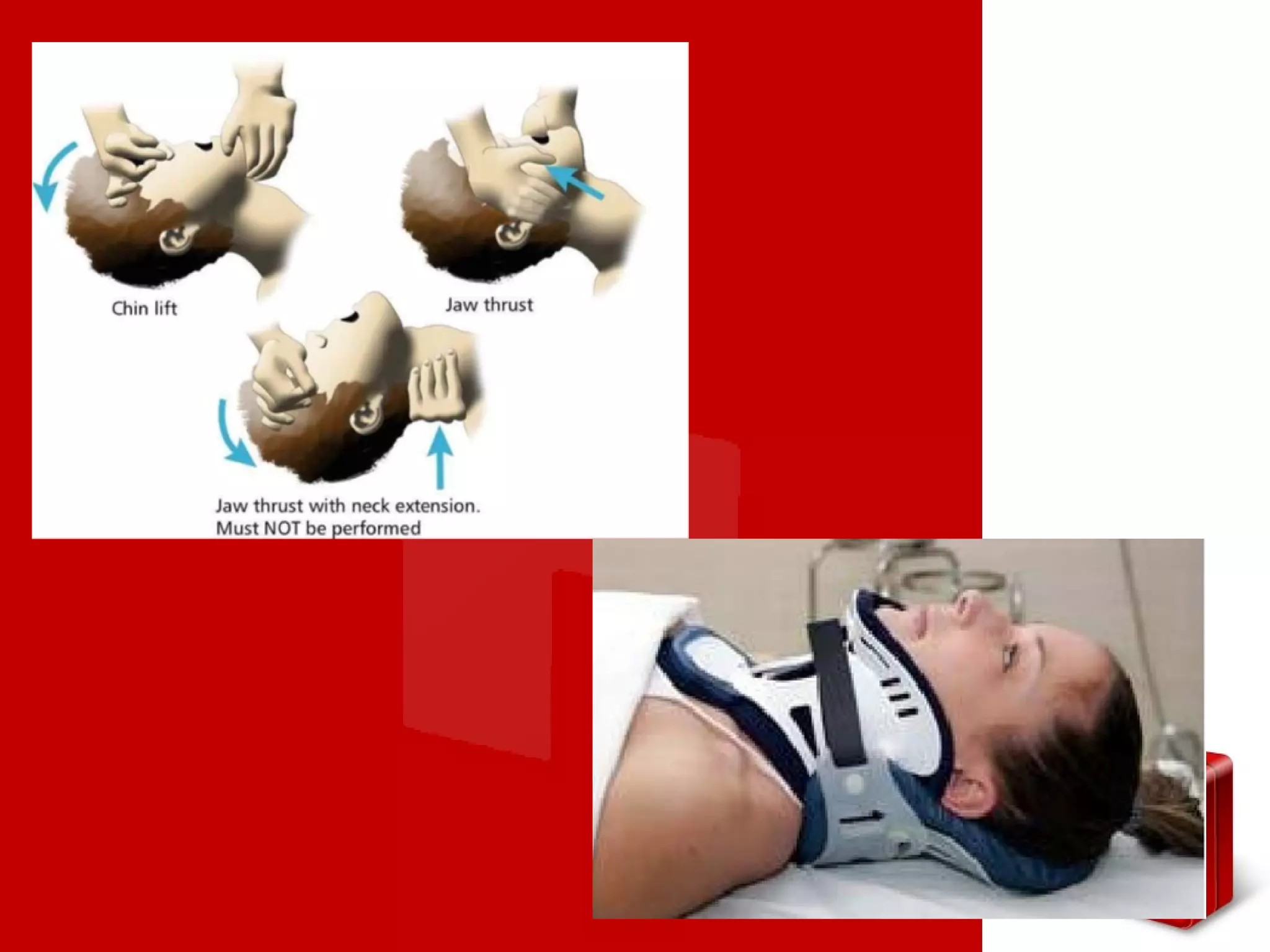
This document outlines the Advanced Trauma Life Support (ATLS) protocol for assessing and treating traumatic patients. It discusses the importance of a standardized approach and maximizing the "golden hour" after trauma. The protocol includes 4 phases: primary survey to address life threats and stabilize the patient, secondary survey for a full physical exam and history, resuscitation, and tertiary survey for comprehensive treatment and stabilization for transfer. Key components of the primary survey are the ABCDE approach to assess airway/cervical spine, breathing, circulation with hemorrhage control, disability, and exposure/environment. The secondary survey involves a full history and head-to-toe physical exam. The goal of tertiary survey is complete treatment