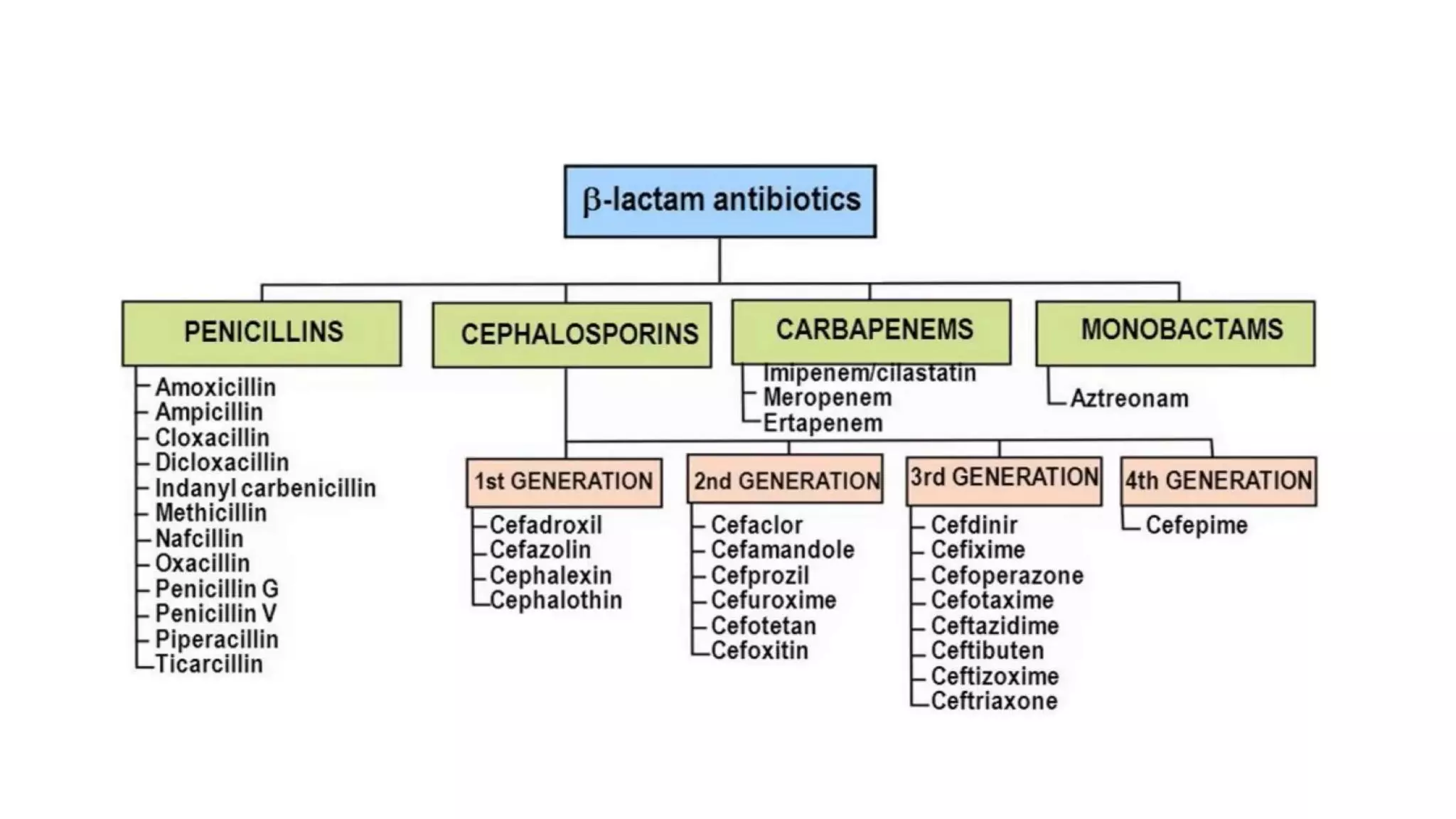
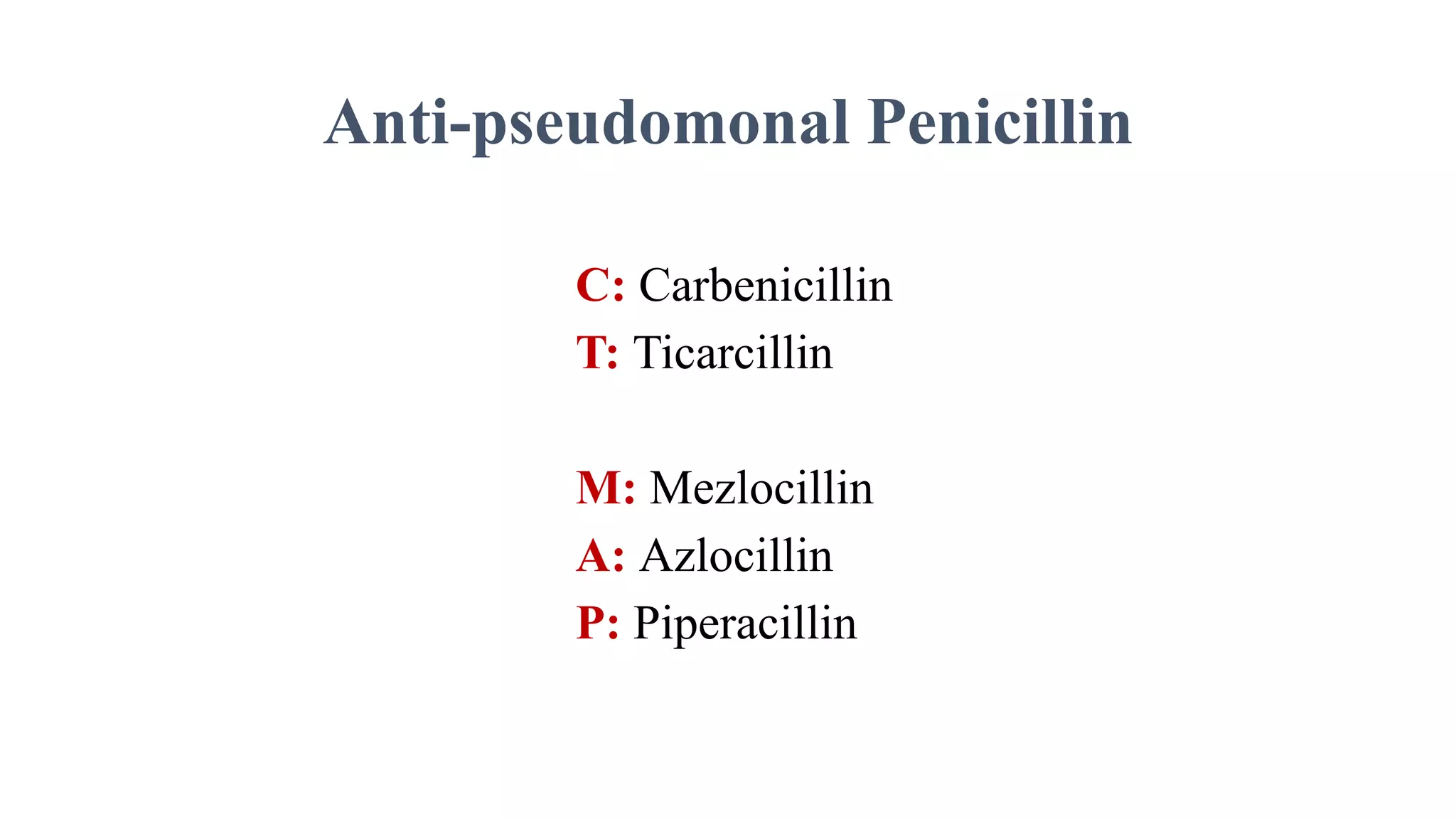
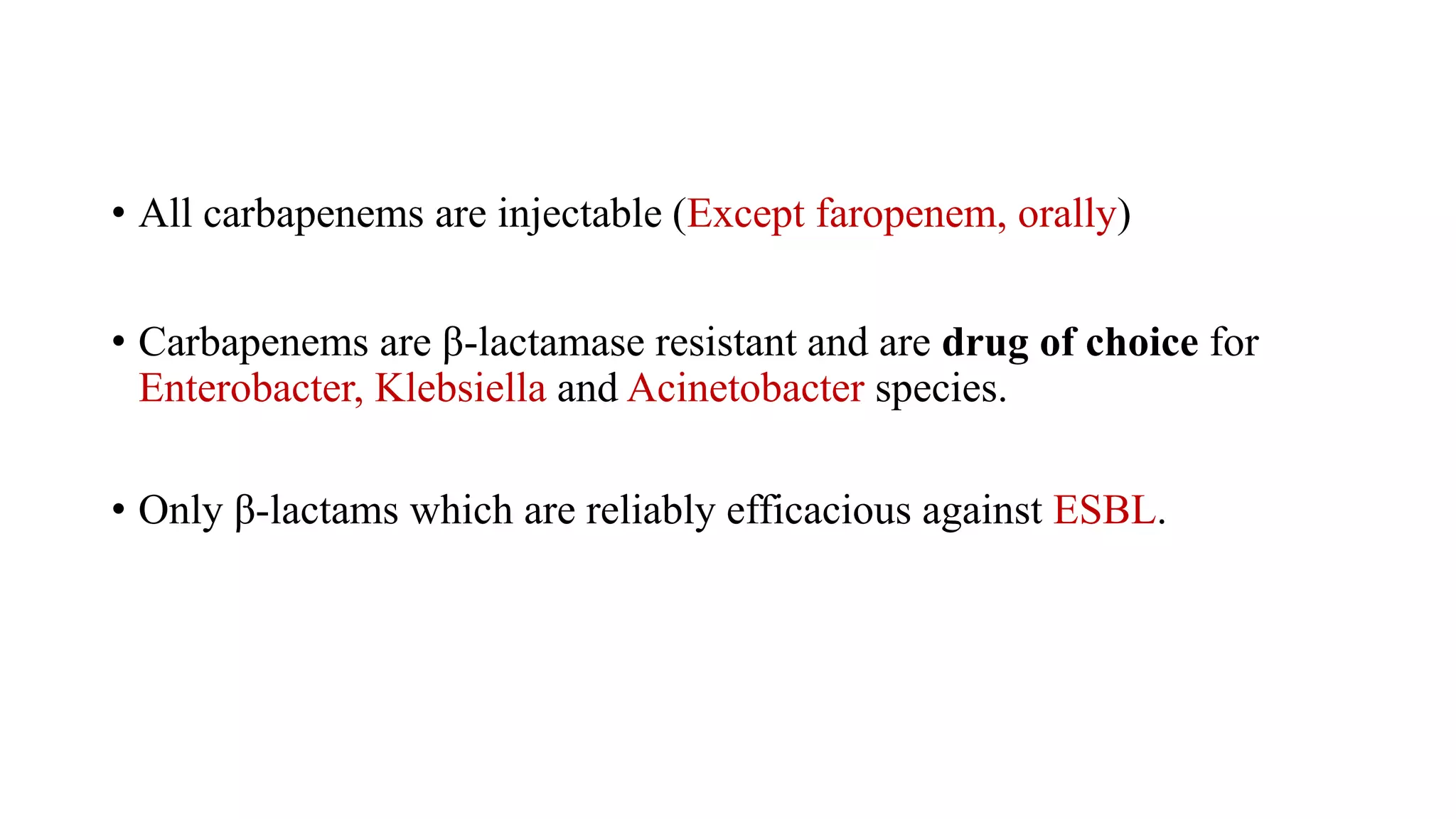
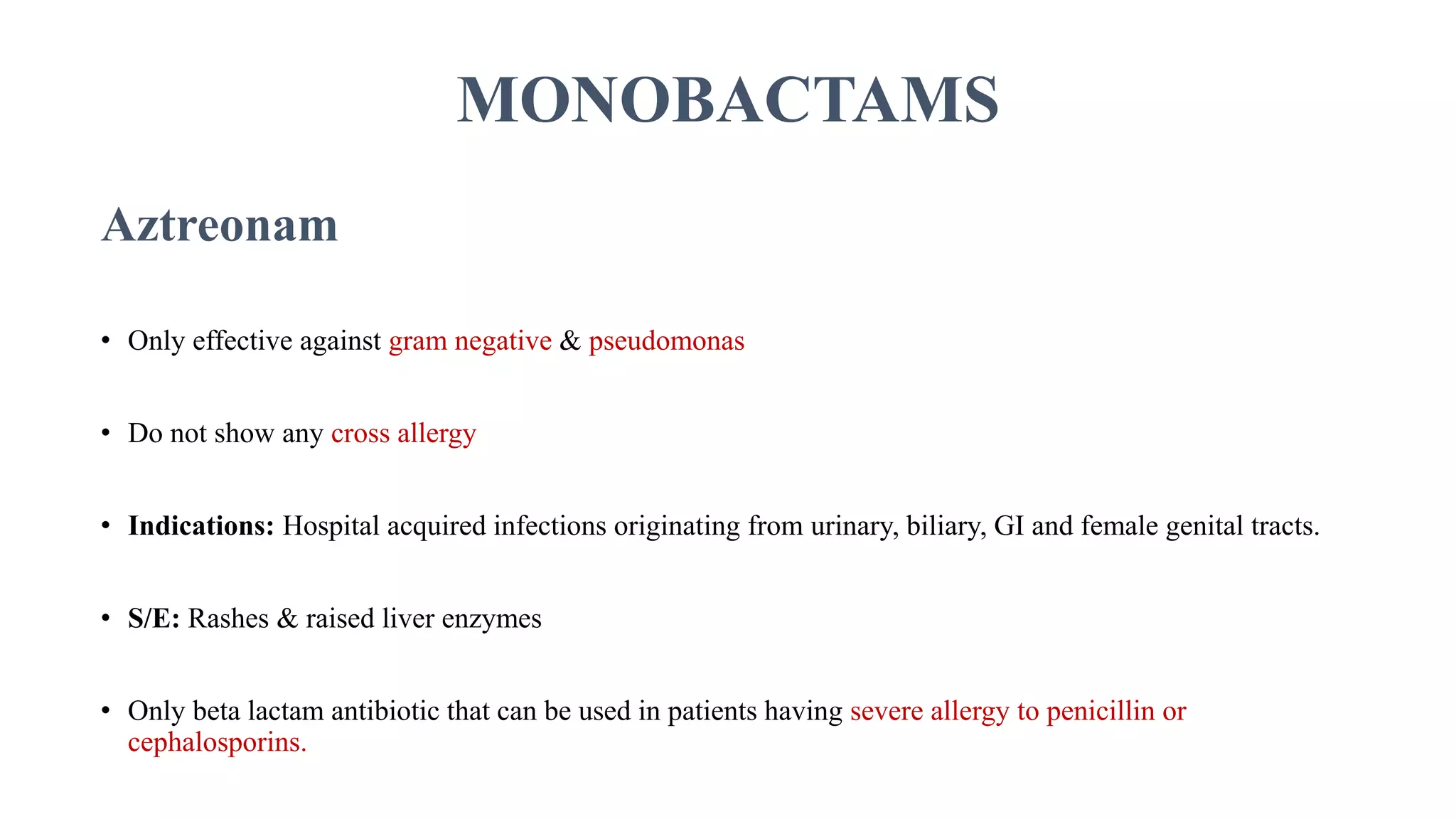
The document provides an extensive overview of beta-lactam antibiotics, detailing various classes such as penicillins, cephalosporins, carbapenems, and monobactams, along with their mechanisms of action, spectrum of activity, and resistance mechanisms. It highlights specific drug combinations, indications for use, and the evolving resistance patterns in bacterial infections. Additionally, it discusses clinical implications in treating conditions like meningitis, typhoid fever, and MRSA, emphasizing the importance of choosing appropriate antibiotics based on susceptibility.