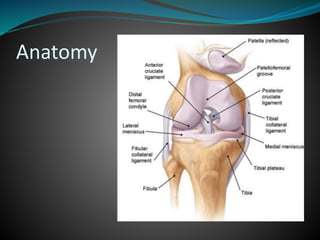
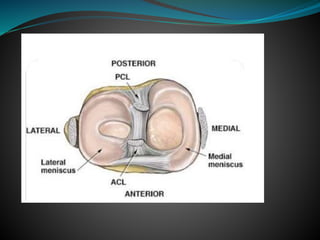
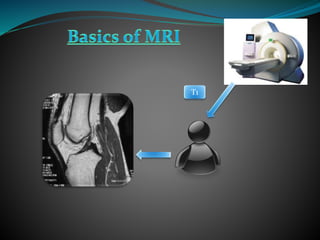
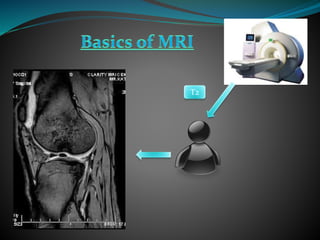
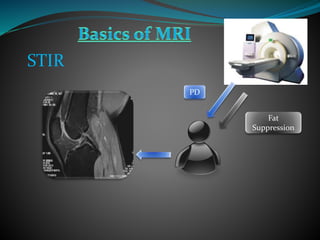
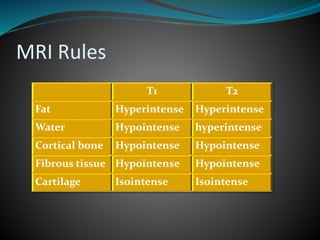
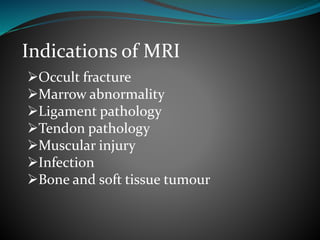
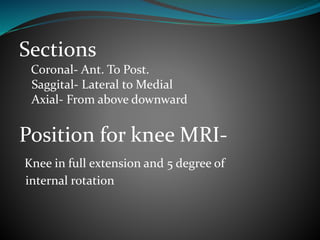
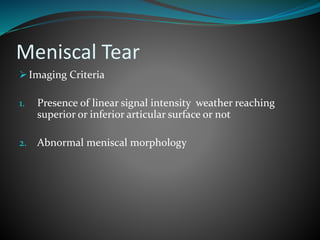
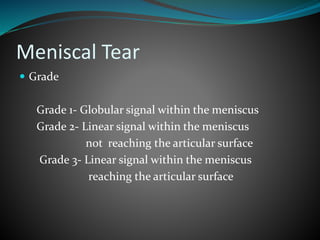
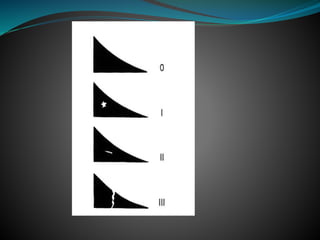
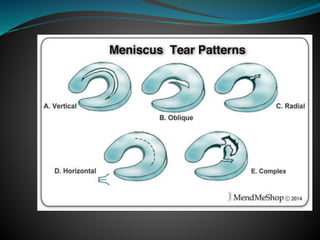
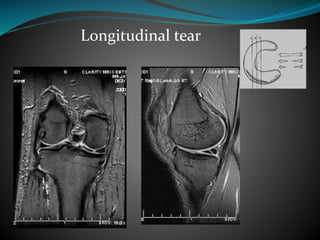
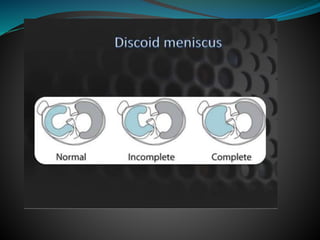
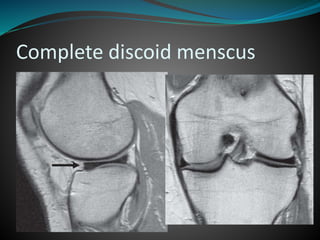
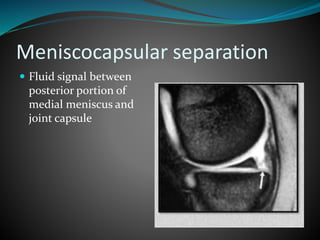
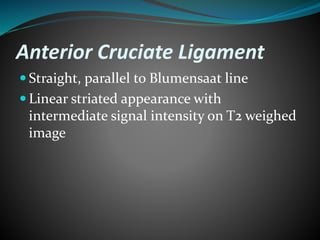
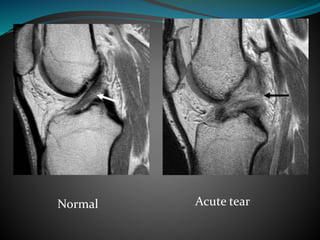
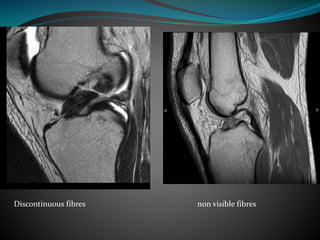
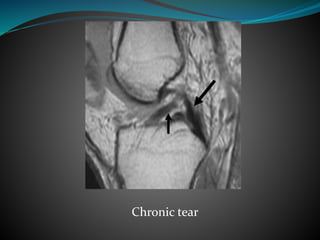
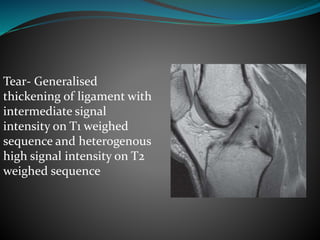
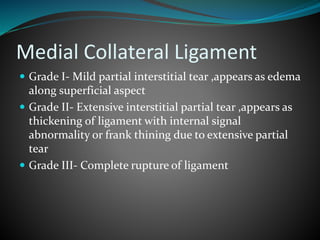
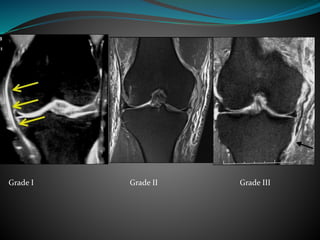
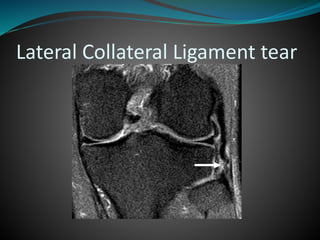
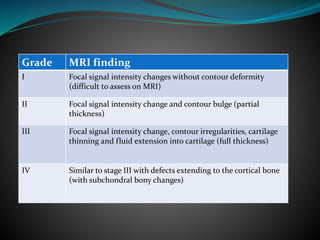
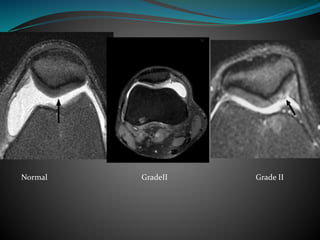
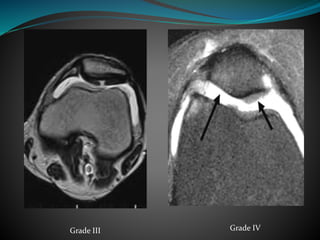
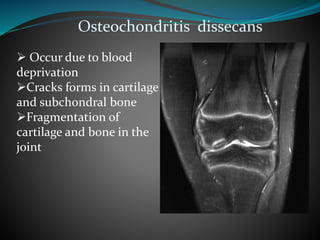
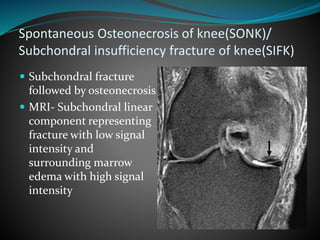
This document provides an overview of MRI techniques and protocols for musculoskeletal imaging. It discusses common musculoskeletal injuries and conditions that can be identified on MRI, including meniscal tears, ligament tears, tendon injuries, osteochondral lesions, and bone marrow abnormalities. For each condition, it describes the MRI appearance and features that help characterize the severity and chronicity of the problem. Images are included to demonstrate the MRI findings for many common orthopedic pathologies.