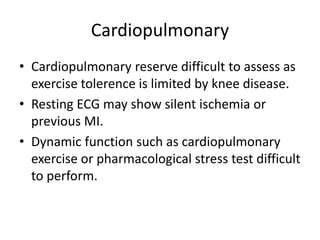
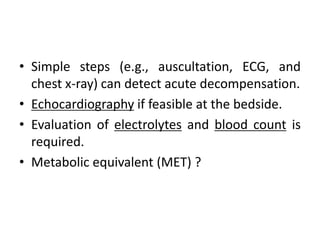
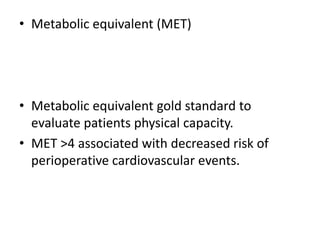
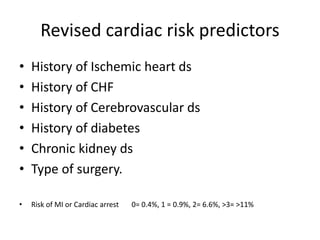
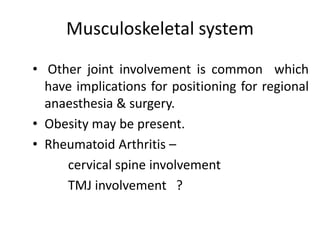
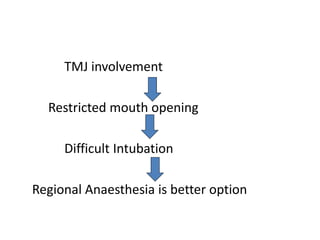
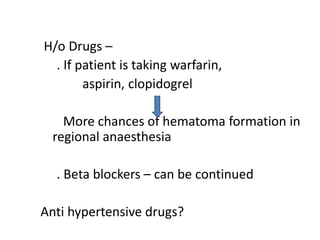
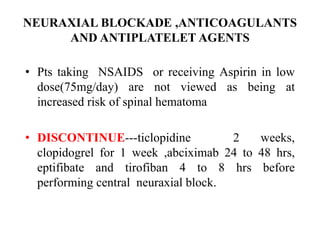
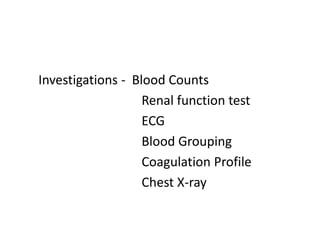
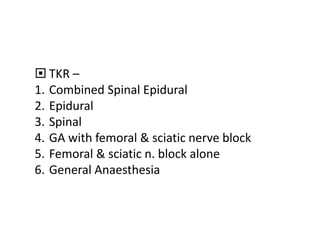
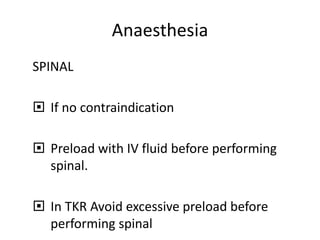
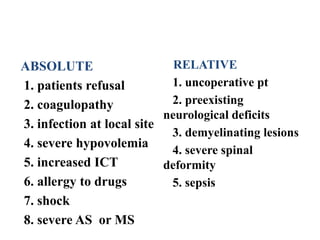
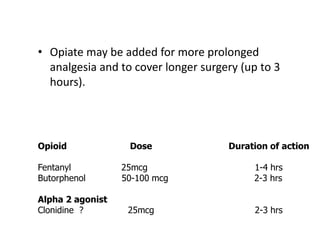
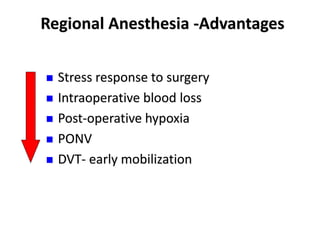
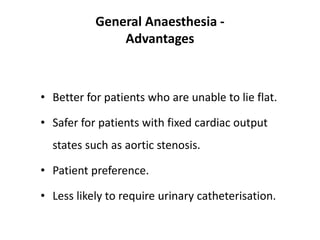
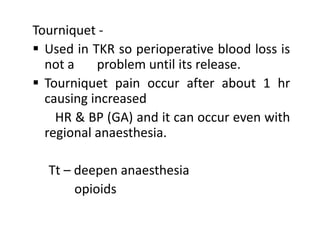
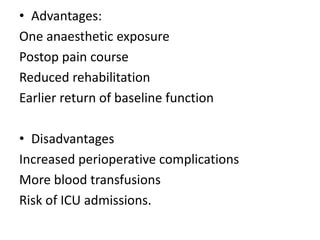
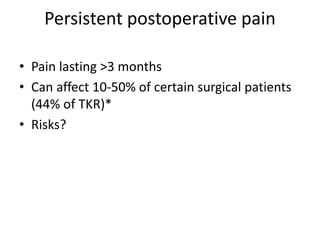
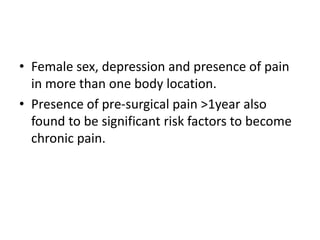
This document discusses anesthesia considerations for total knee replacement (TKR) surgery. It covers preoperative evaluation of cardiopulmonary and musculoskeletal systems, anesthesia techniques including spinal, epidural, peripheral nerve blocks and general anesthesia, intraoperative monitoring and tourniquet use, postoperative care including pain management, and complications associated with TKR such as blood loss, infection and venous thromboembolism. Regional anesthesia techniques are preferred due to advantages like less blood loss, better pain control and early mobilization, though patient factors and surgical needs determine the best option.