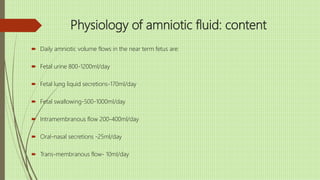
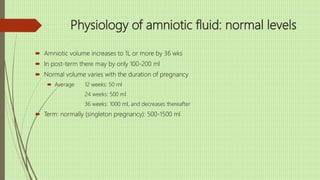
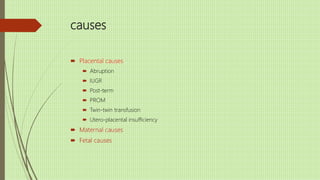
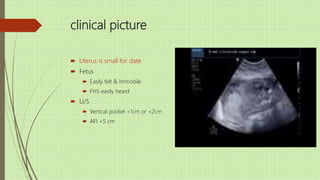
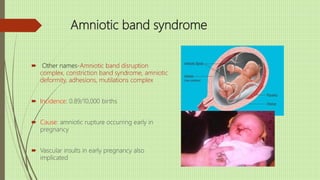
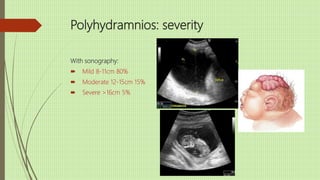
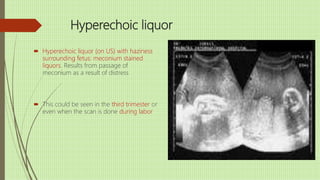
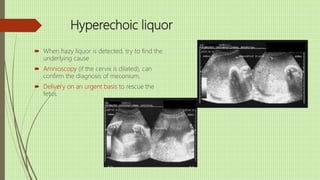
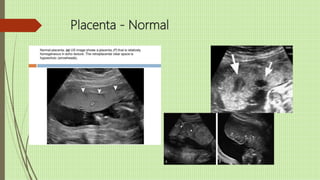
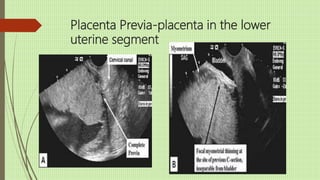
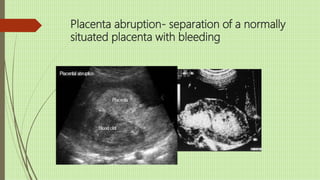
The document discusses the importance of third trimester scanning for assessing fetal health, placenta, and amniotic fluid conditions. It covers various abnormalities such as oligohydramnios and polyhydramnios, their causes, clinical features, and consequences on fetal well-being. It emphasizes the role of ultrasound in diagnosing these conditions and outlines potential treatment options and complications associated with each condition.