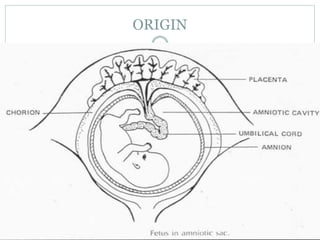
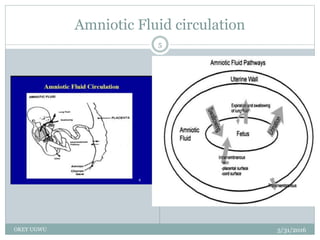
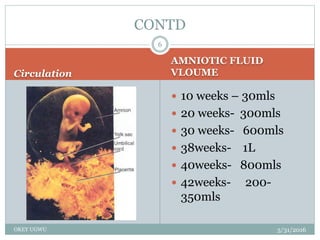
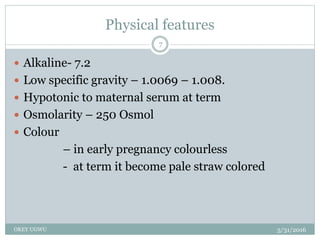
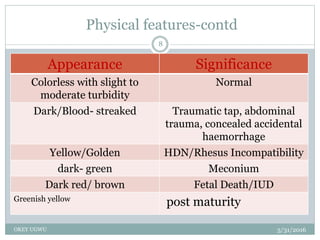
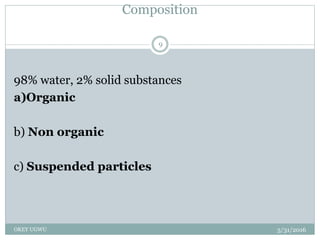
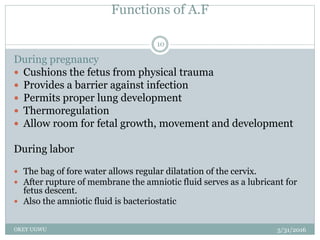
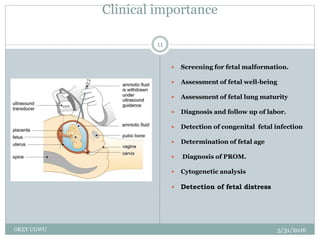
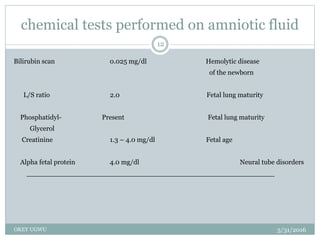
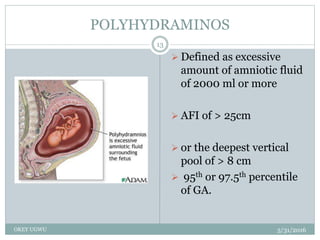
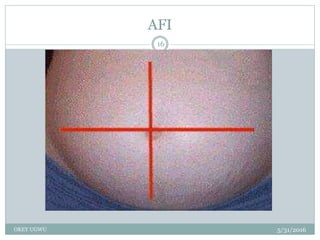
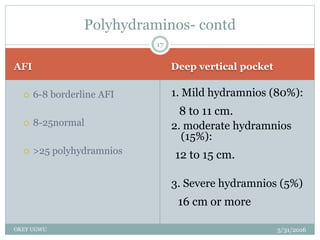
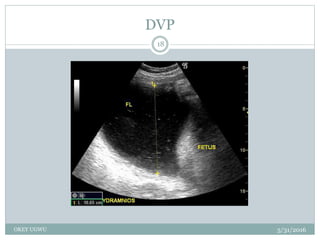
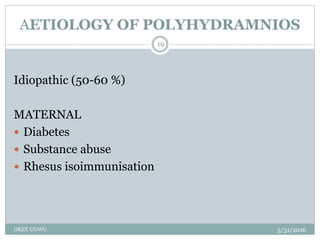
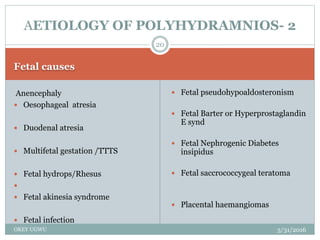
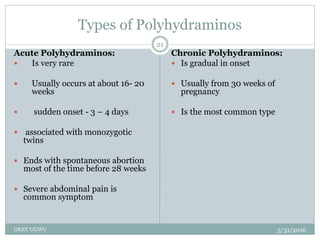
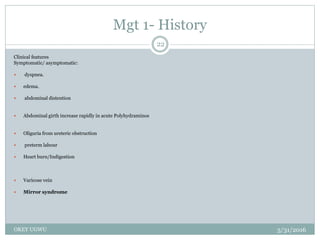
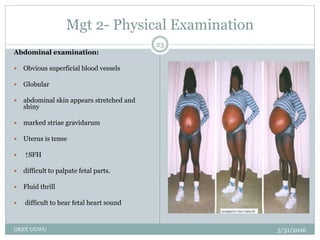
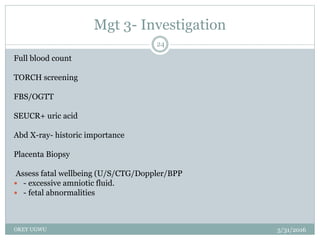
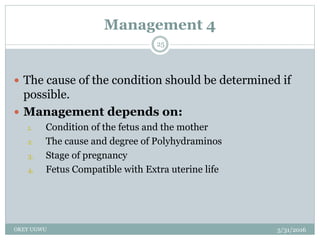
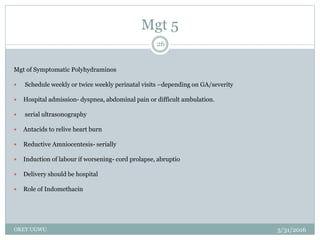
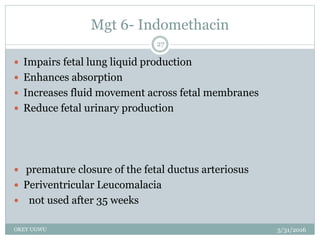
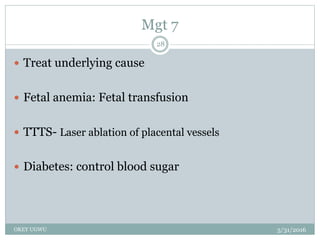
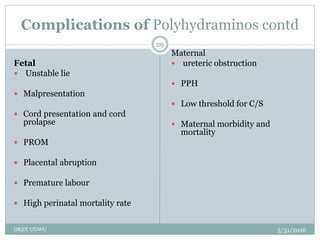
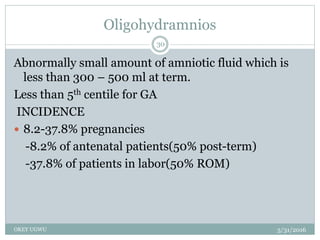
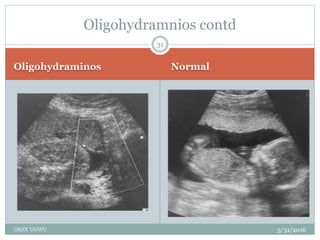
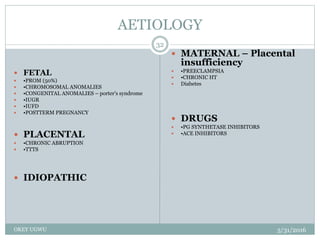
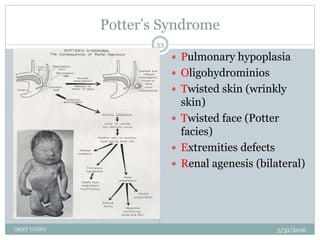
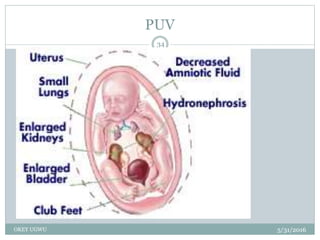
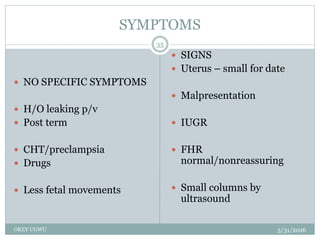
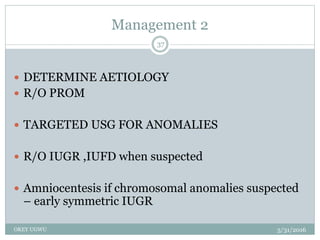
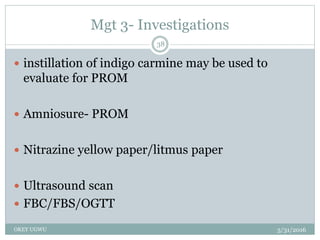
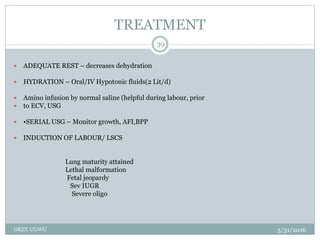
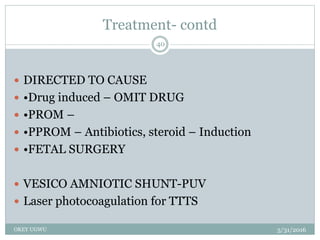
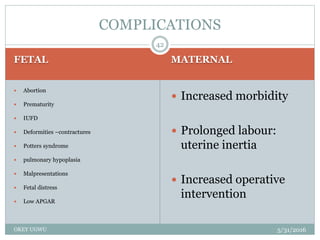
This document discusses disorders of amniotic fluid volume, including oligohydramnios and polyhydramnios. It begins by describing the origin, circulation, physical features and components of normal amniotic fluid. It then defines oligohydramnios and polyhydramnios, discusses their causes, clinical presentation, diagnostic evaluation and management. Complications are also outlined. The document provides detailed information on the etiology, investigations and treatment of the two conditions. It emphasizes that oligohydramnios is associated with high rates of pulmonary hypoplasia, growth restriction and adverse pregnancy outcomes.