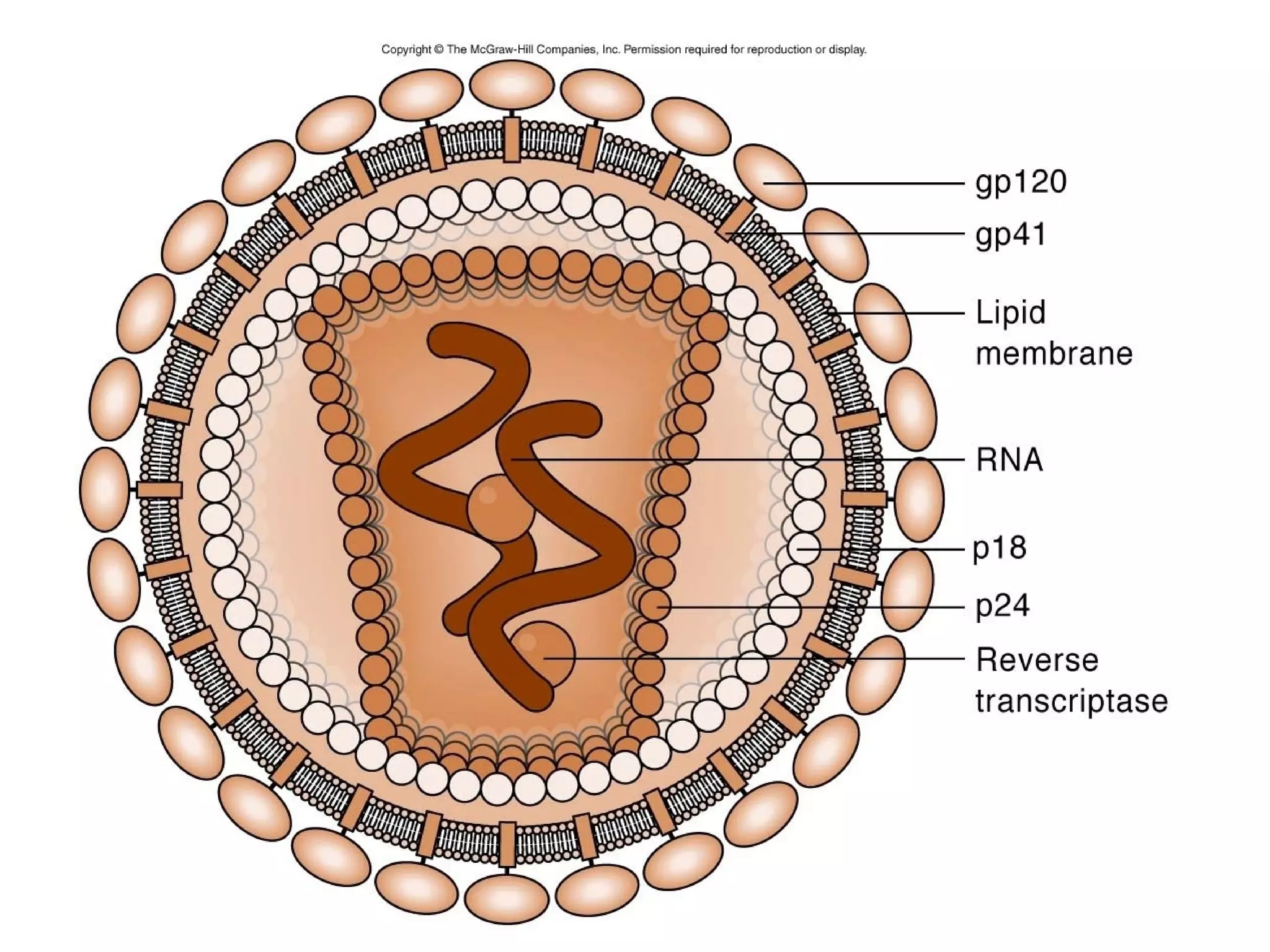
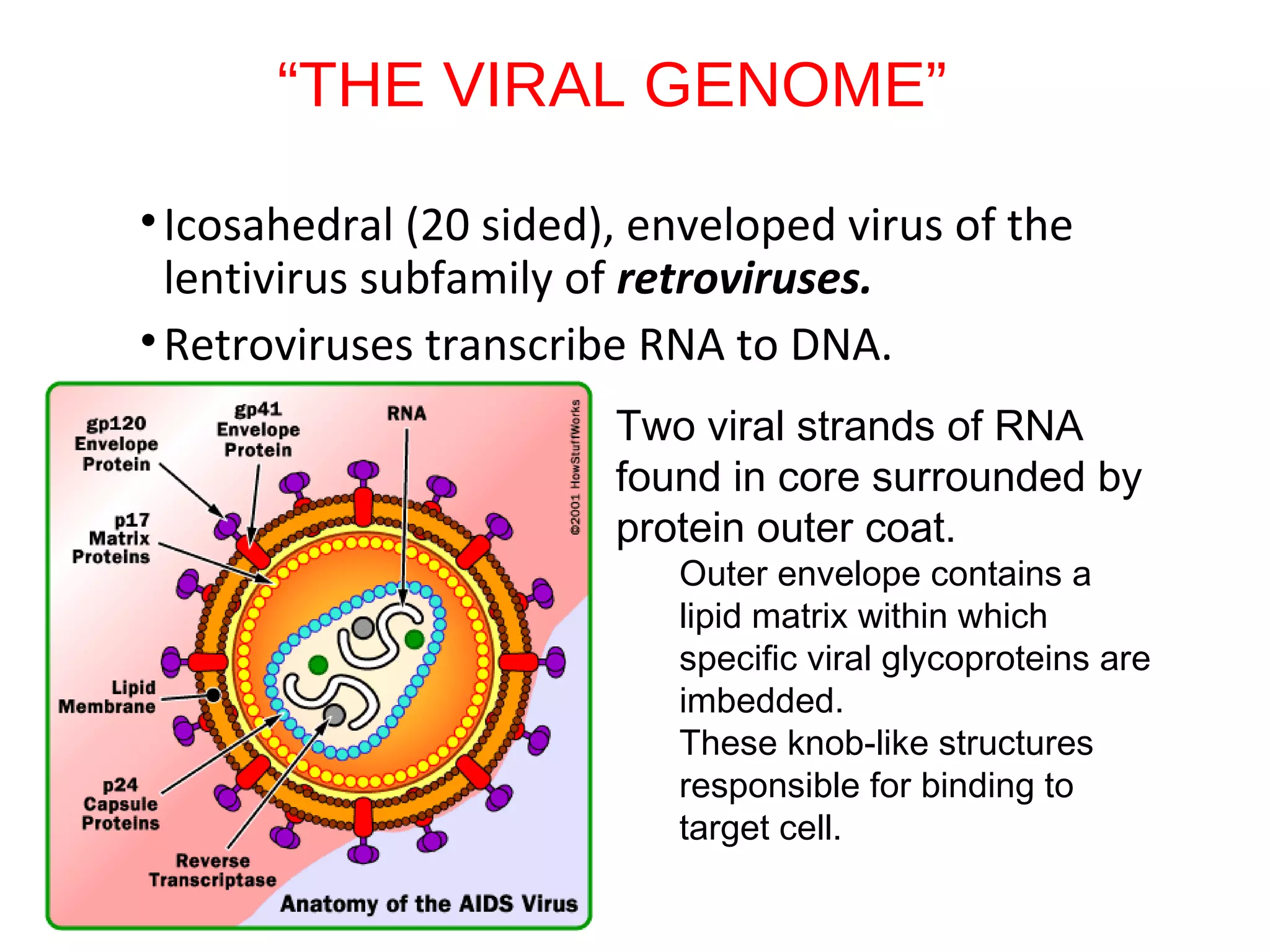
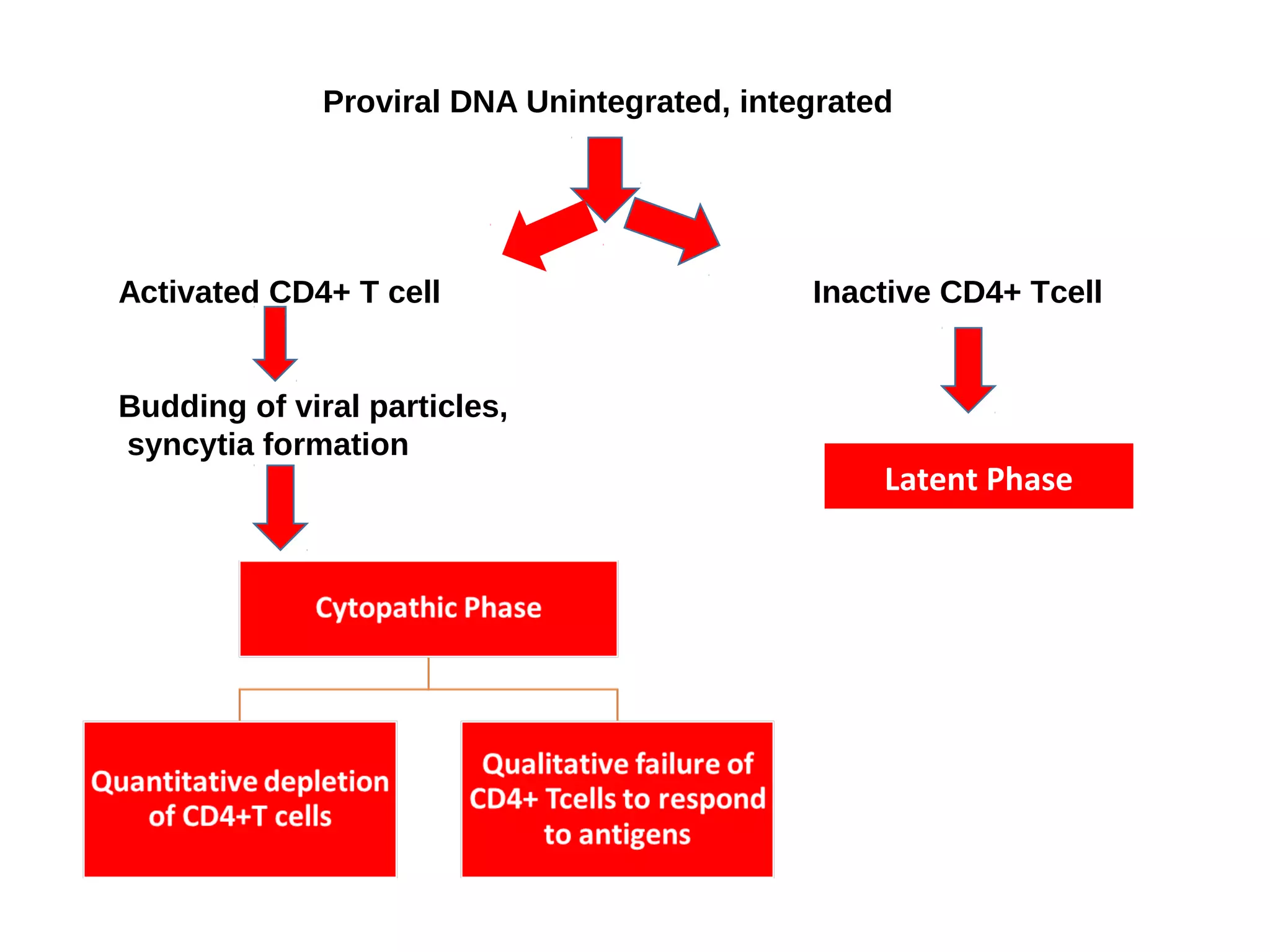
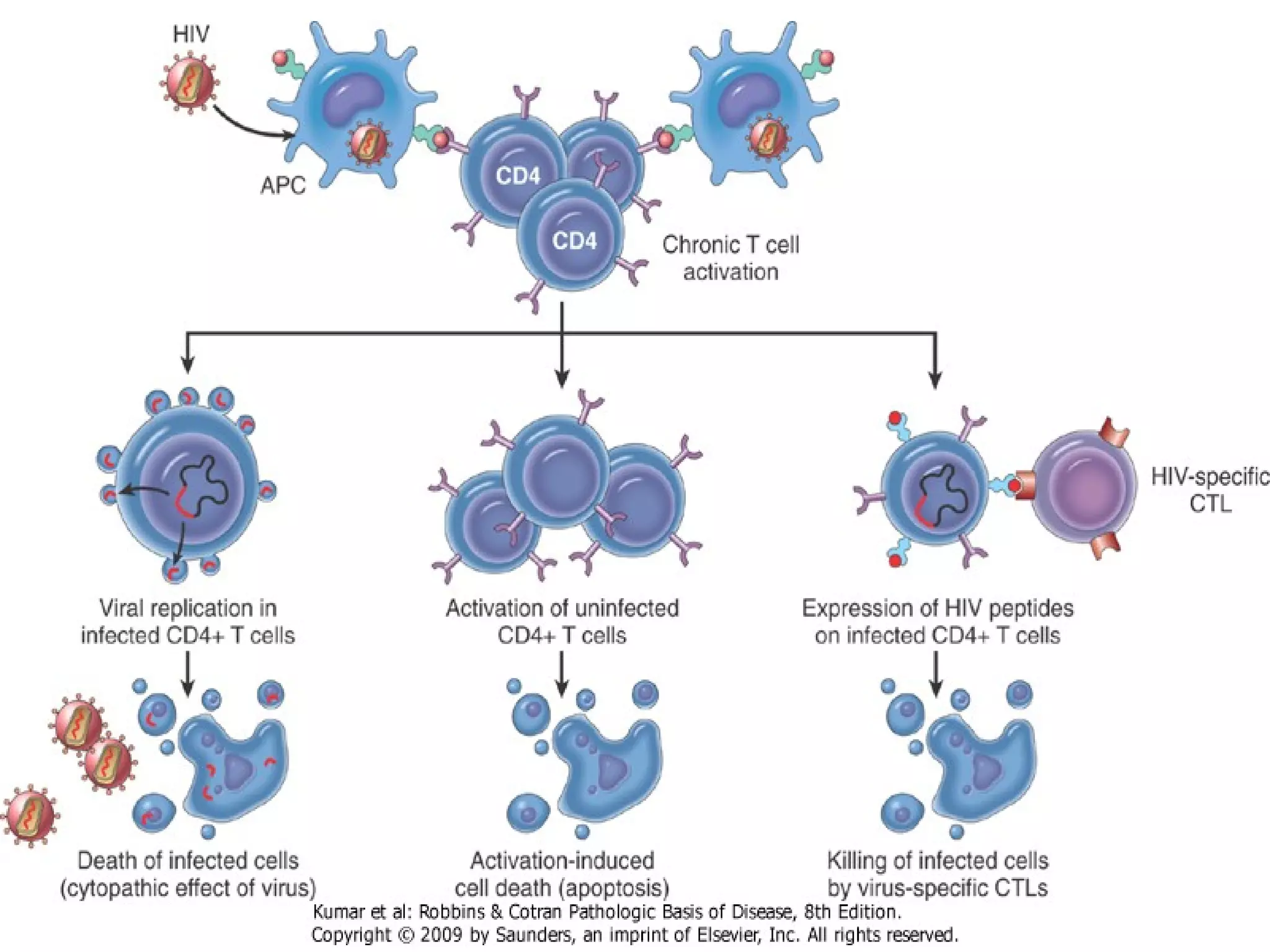
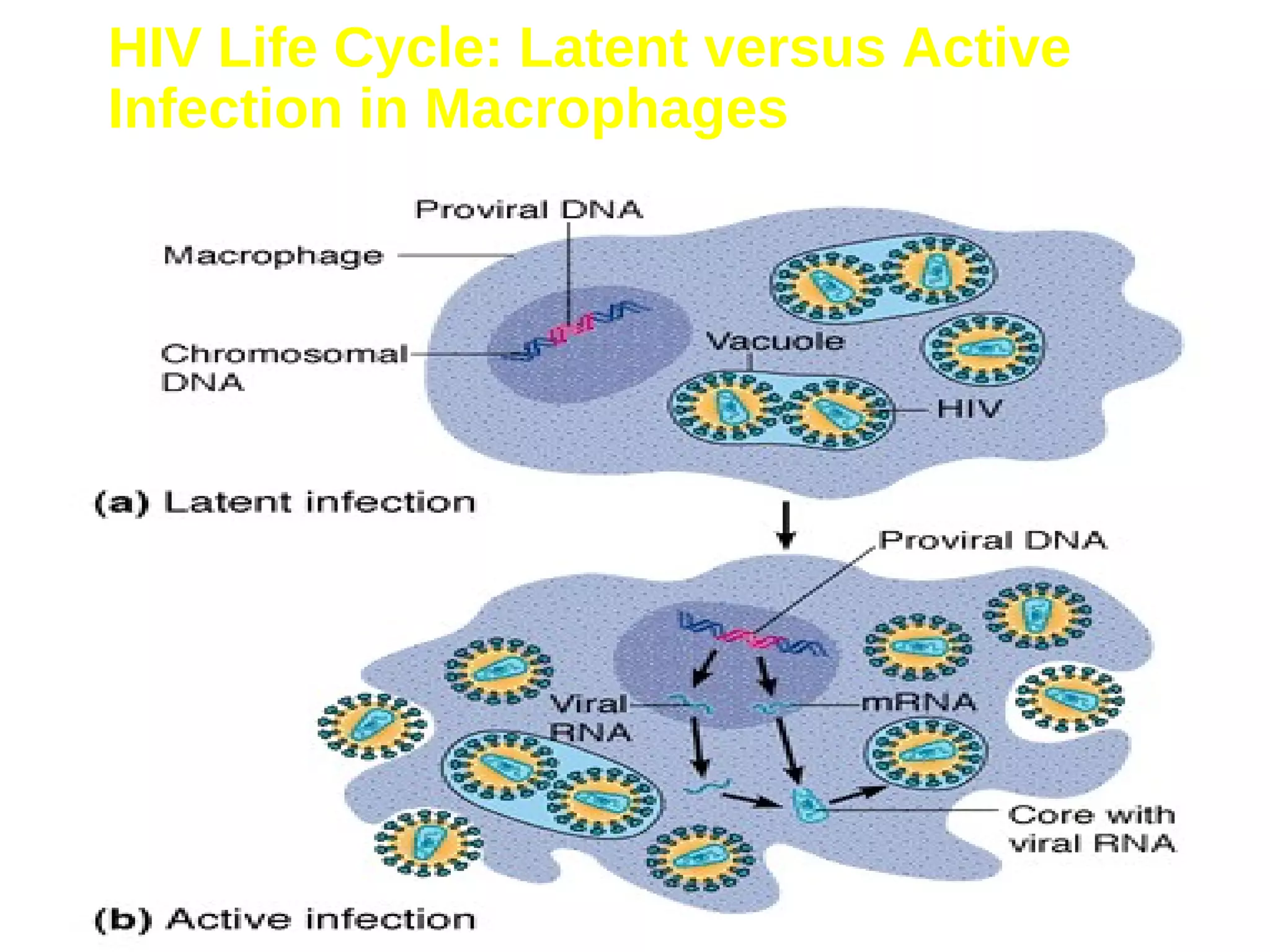
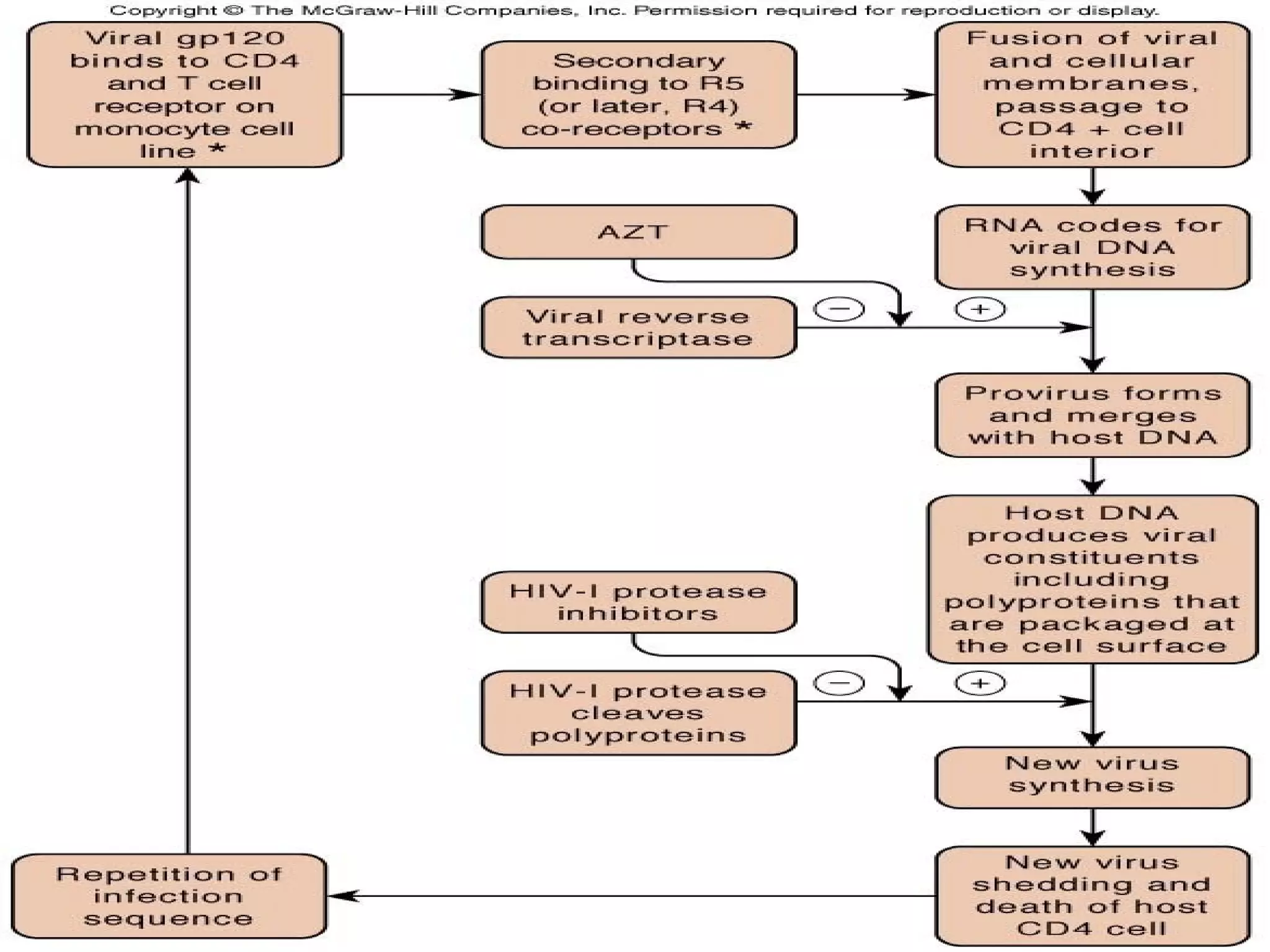
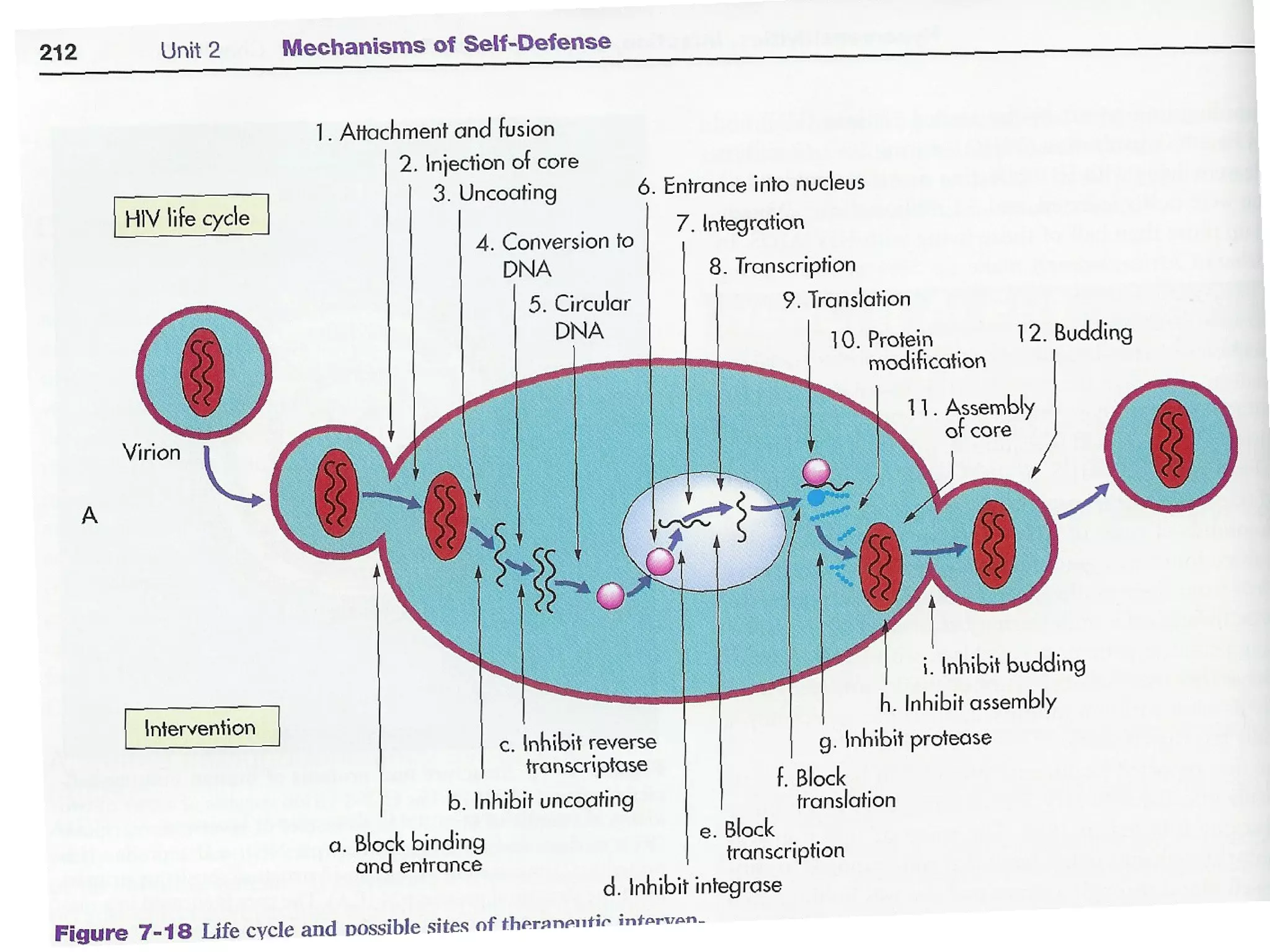
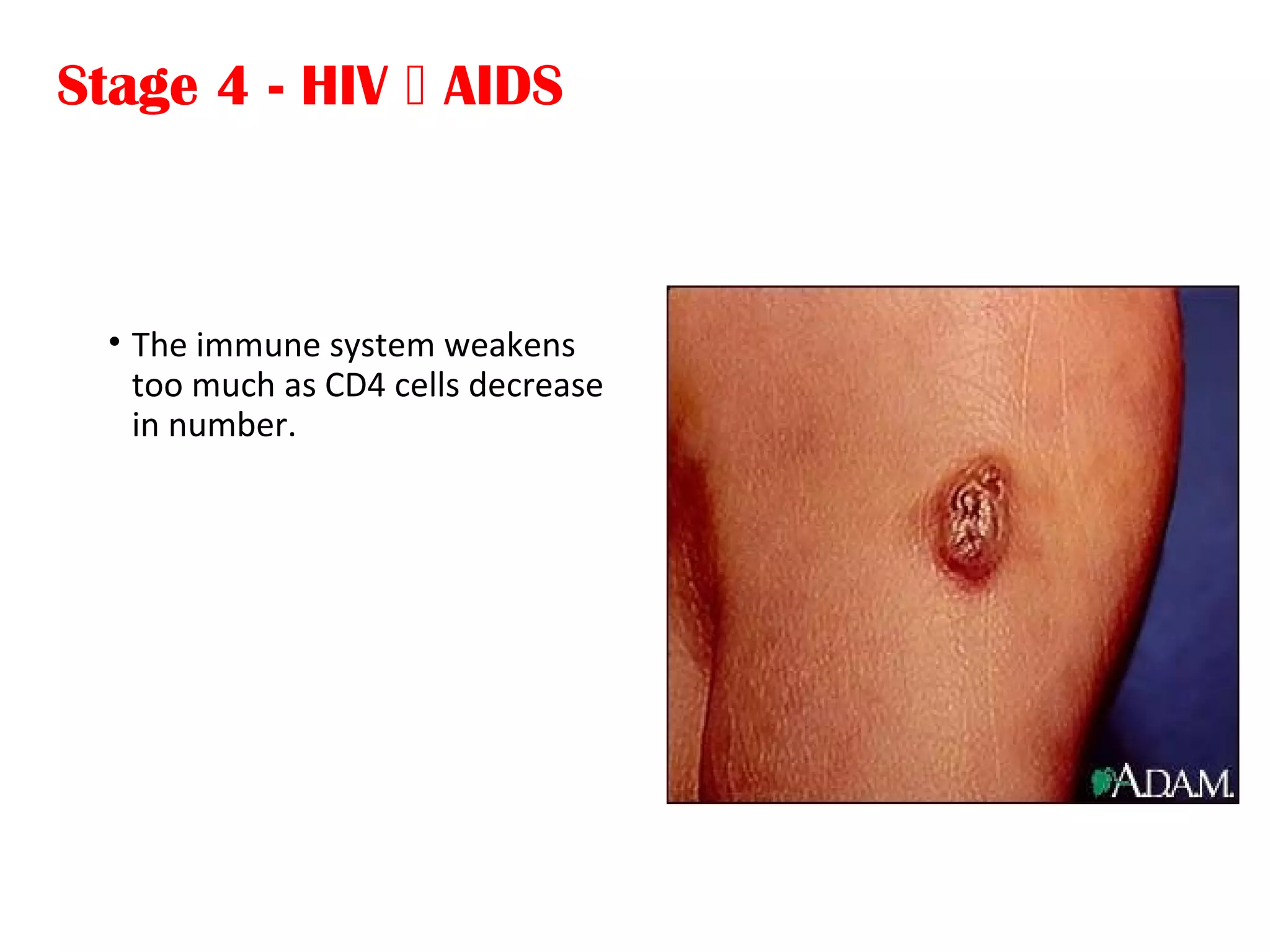
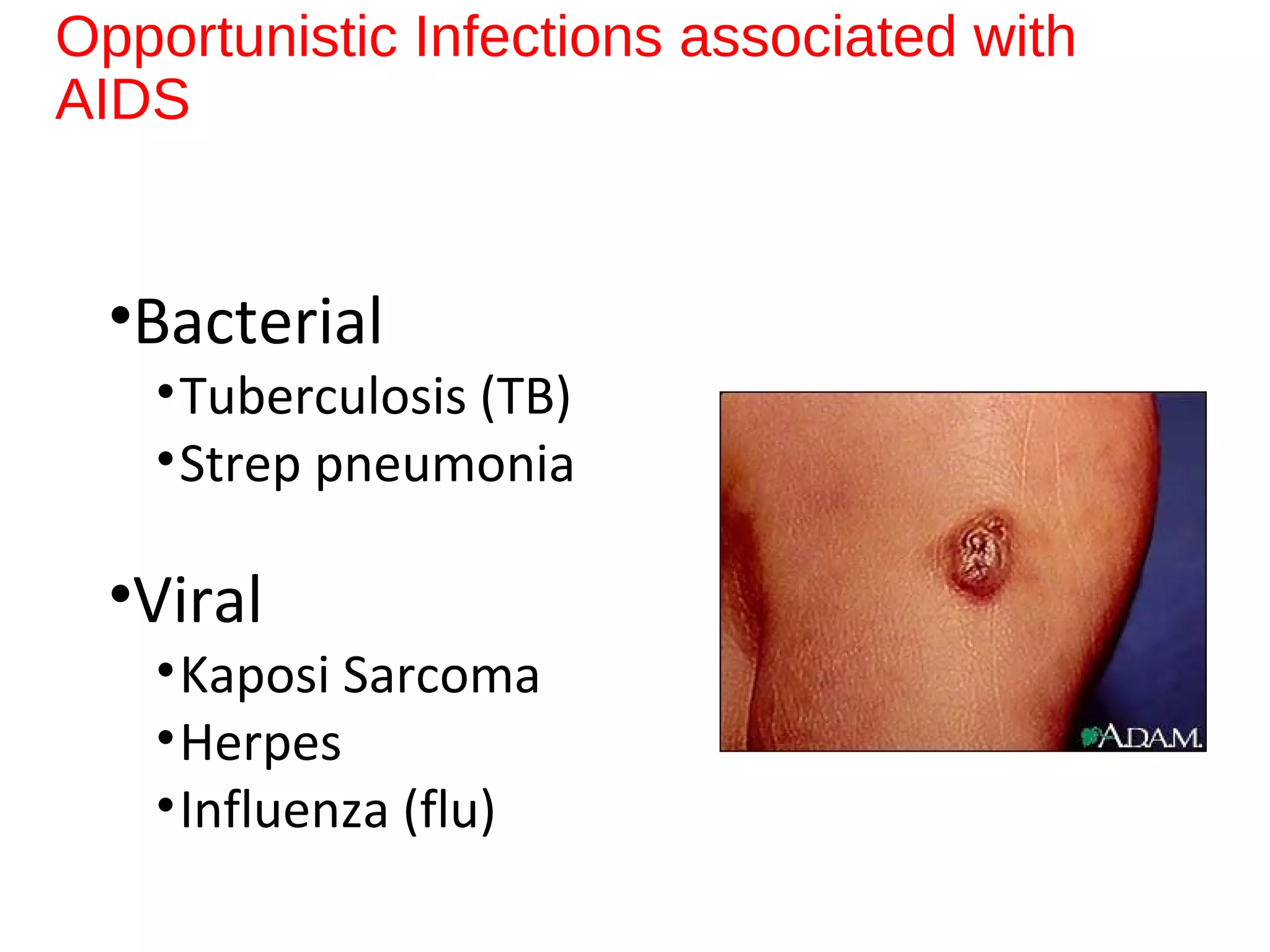
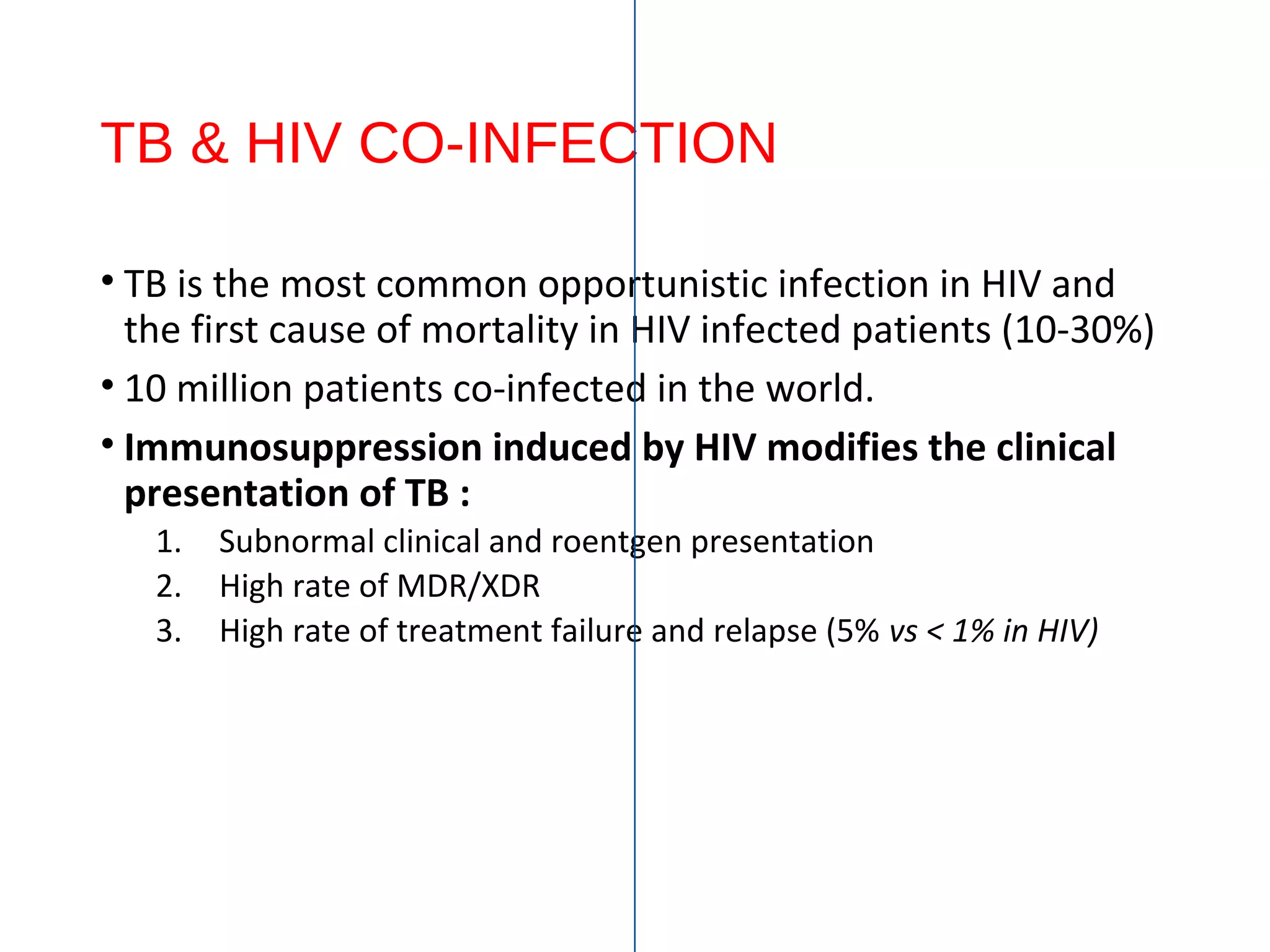
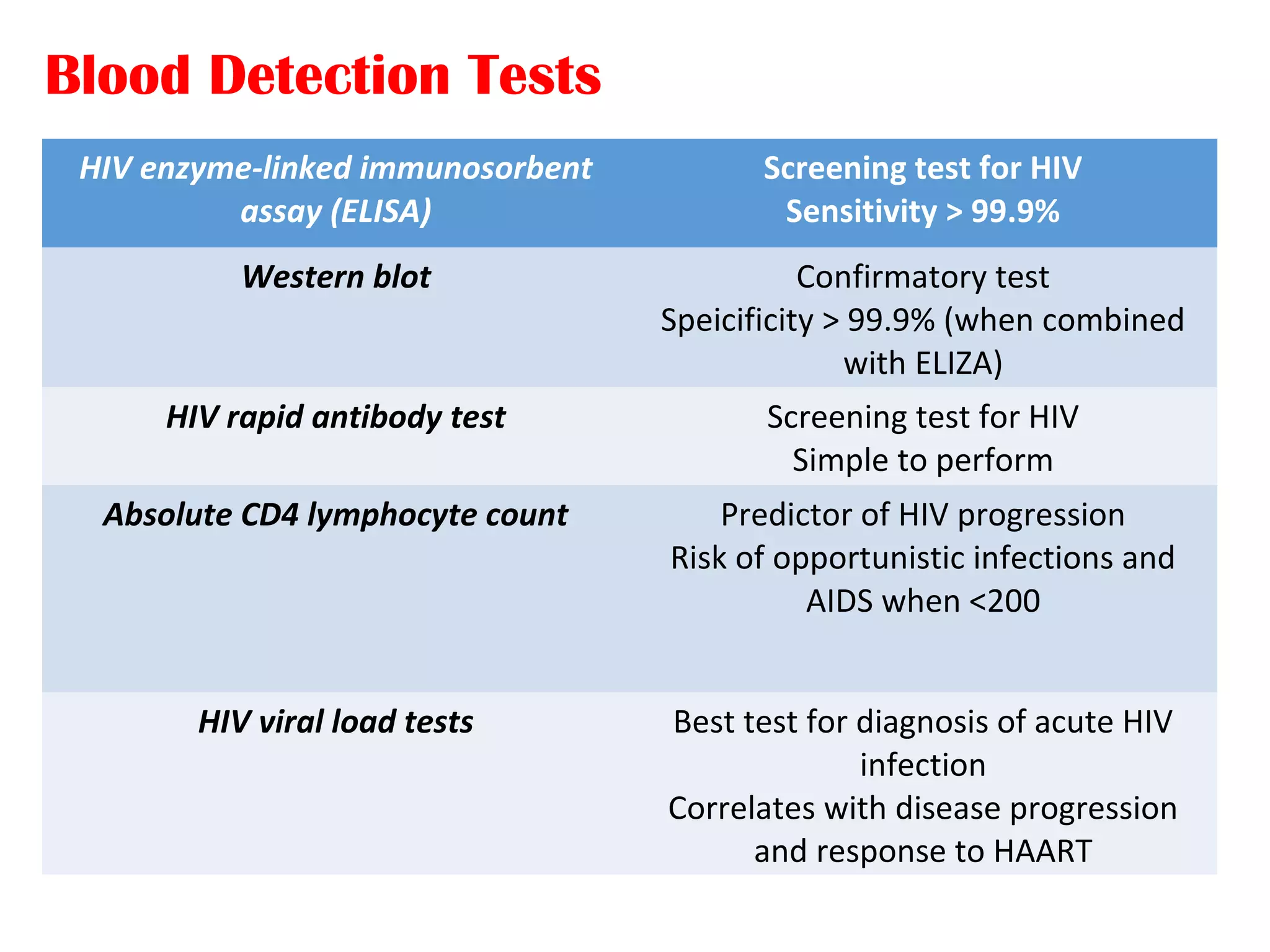
Acquired immunodeficiency syndrome (AIDS) is caused by the human immunodeficiency virus (HIV) which impairs the immune system. HIV specifically targets CD4+ T cells (helper T cells). The virus can be transmitted through bodily fluids like blood, semen, vaginal fluids. The natural course of HIV infection progresses from primary infection with flu-like symptoms, to asymptomatic latency period that can last 10 years, to symptomatic stage as the immune system deteriorates, and finally AIDS when opportunistic infections take hold. While there is no cure for HIV/AIDS, antiretroviral treatment can control the virus and prevent transmission.