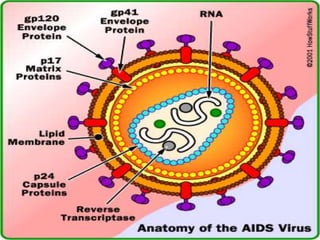
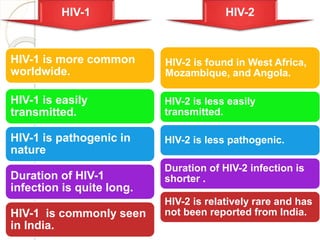
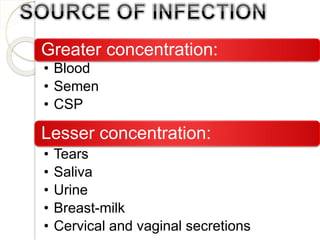
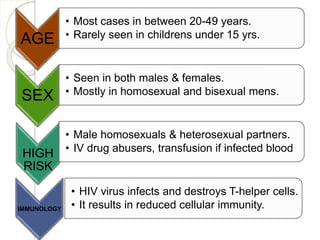
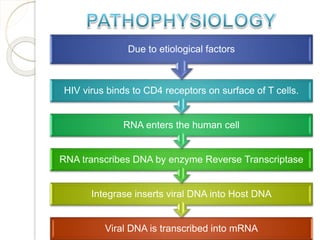
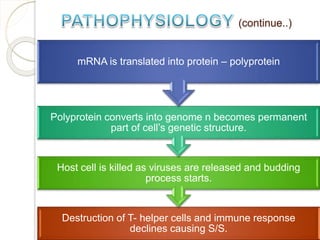
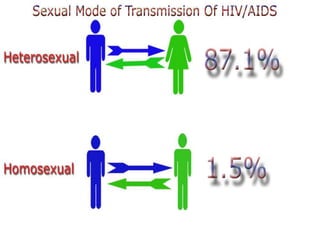
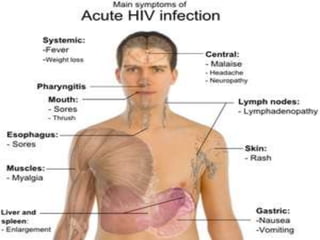
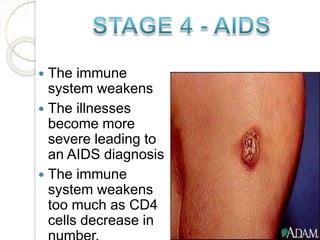
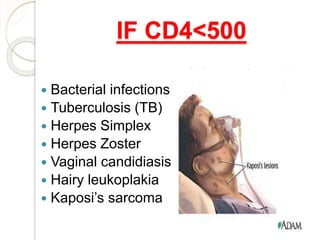
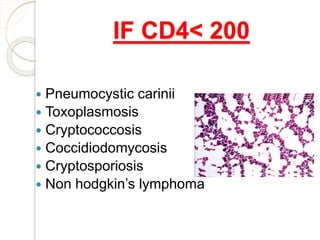
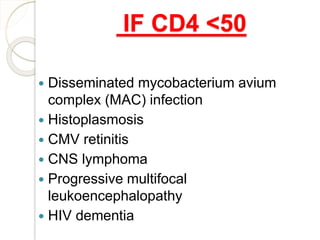
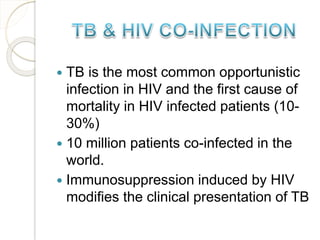
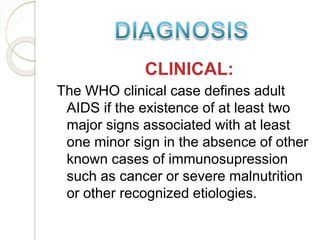
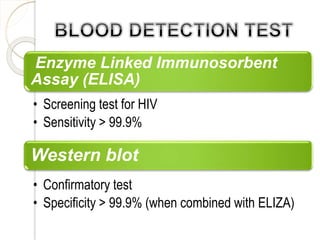
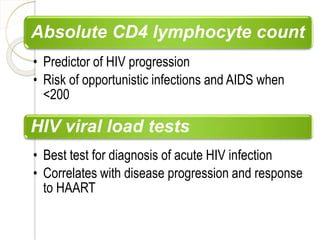
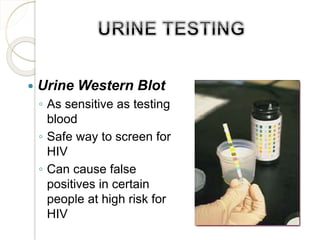
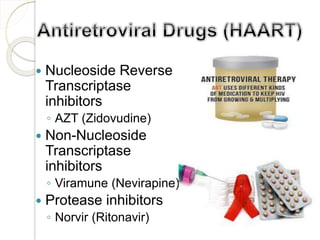
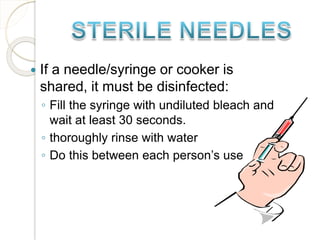
The document discusses HIV/AIDS, describing what each abbreviation stands for and providing details about the virus, how it is transmitted, stages of infection, opportunistic infections, screening tests, treatment, and prevention methods. It defines HIV as a virus that weakens the immune system and AIDS as the late stage where opportunistic infections take hold. Transmission occurs via blood, semen, vaginal and cervical fluids mainly through unprotected sex and sharing of needles. Prevention includes abstinence, monogamy, condom use, and clean needles.