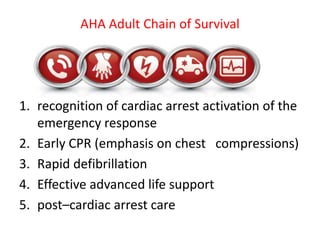
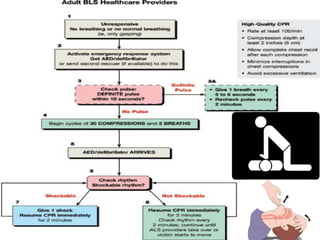
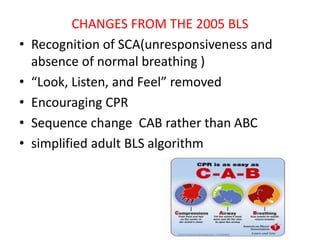
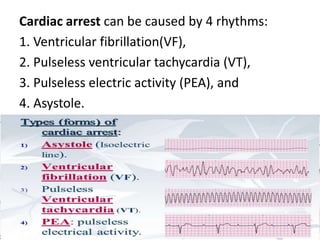
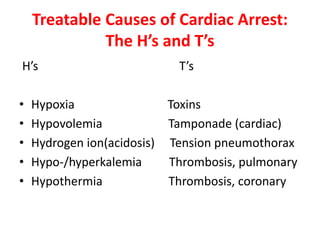
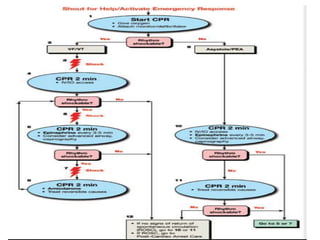
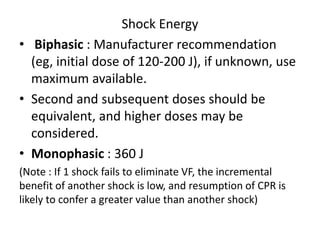
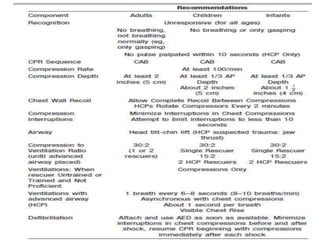
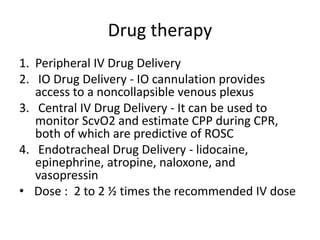
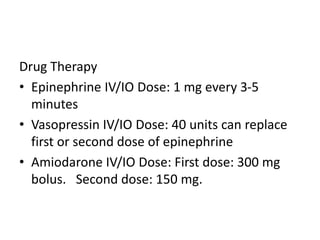
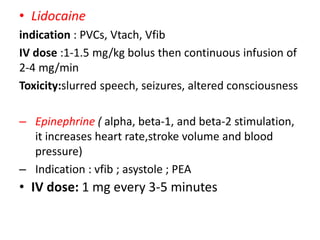
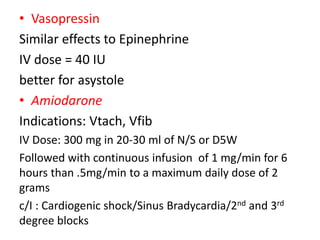
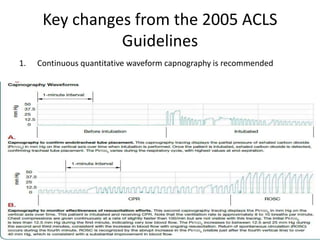
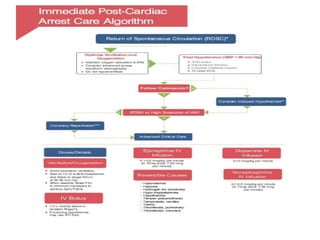
This document provides an overview of Advanced Cardiac Life Support (ACLS). It discusses interventions to prevent cardiac arrest, treat cardiac arrest, and improve outcomes for those who experience return of spontaneous circulation after cardiac arrest. The key elements of the adult chain of survival are recognition, early CPR, rapid defibrillation, effective advanced life support, and post-cardiac arrest care. Causes of cardiac arrest include ventricular fibrillation, pulseless ventricular tachycardia, pulseless electric activity, and asystole. Drug therapies and their dosages are outlined, including epinephrine, vasopressin, amiodarone, and lidocaine. Key changes from 2005 ACLS guidelines include the use of continuous quantitative