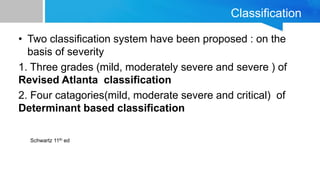
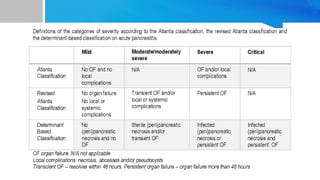
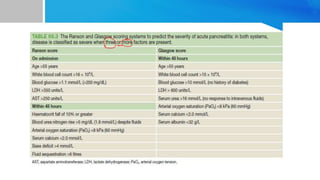
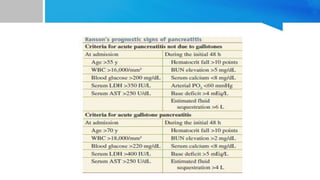
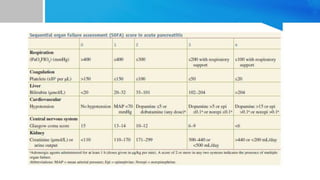
This document provides an overview of acute pancreatitis including its anatomy, etiology, pathophysiology, diagnosis, severity assessment, treatment, and complications. Some key points:
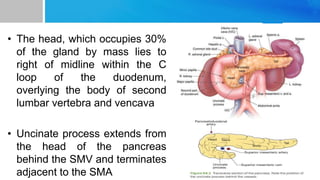
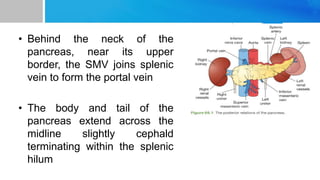
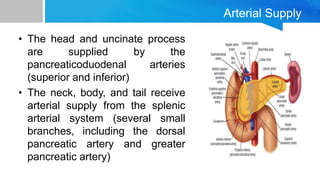
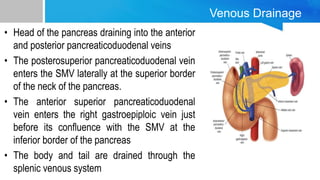
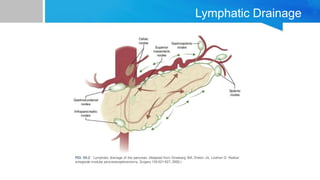
- The pancreas is located in the retroperitoneum and has a head, neck, body and tail supplied by various arteries and veins.
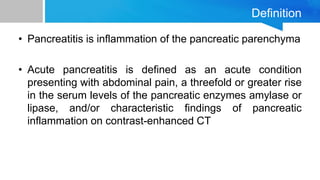
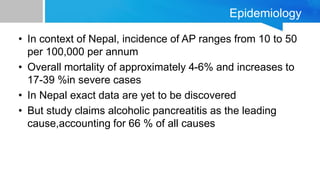
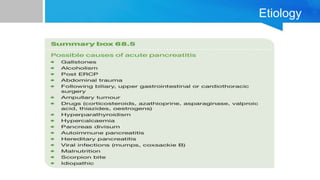
- Acute pancreatitis is defined as inflammation of the pancreas with abdominal pain and elevated pancreatic enzymes. Common causes include gallstones, alcohol use, and hyperlipidemia.
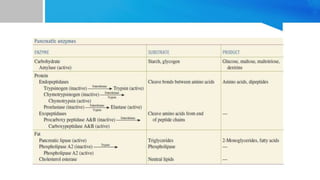
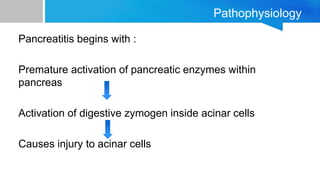
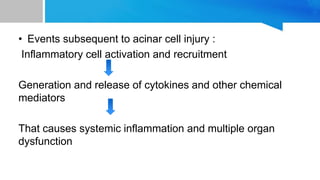
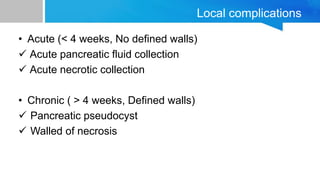
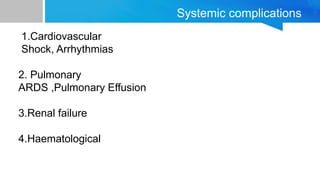
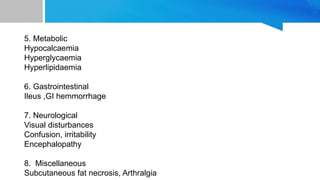
- Inflammation occurs when pancreatic enzymes prematurely activate within the pancreas, causing injury. Systemic complications can develop depending on severity.
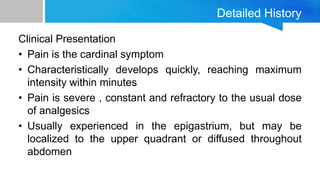
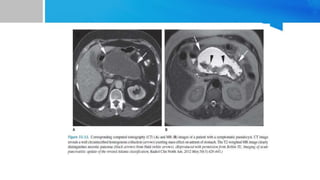
- Diagnosis involves history, exam, and lab tests