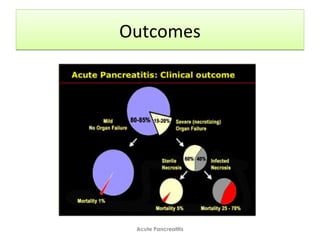
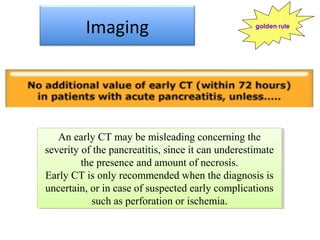
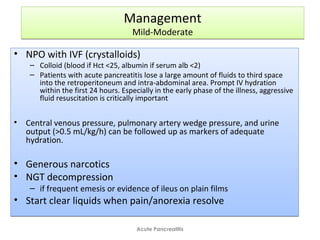
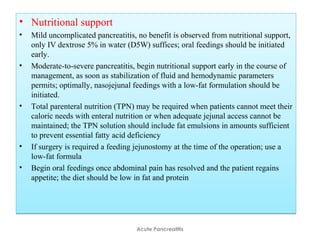
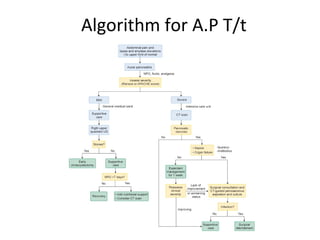
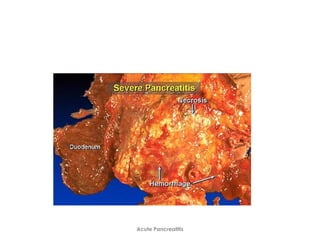
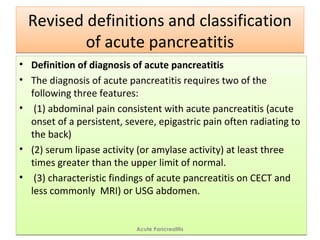
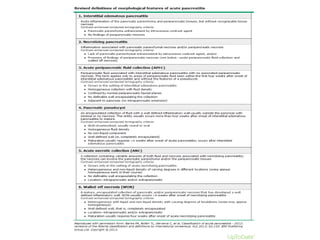
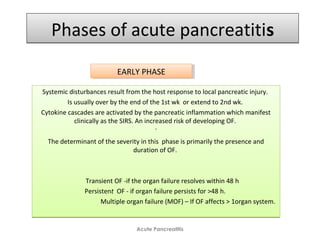
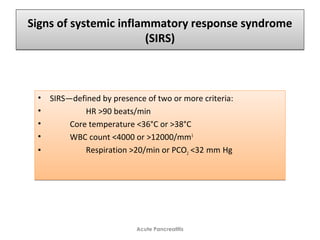
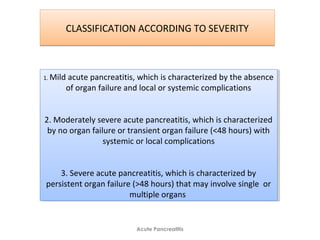
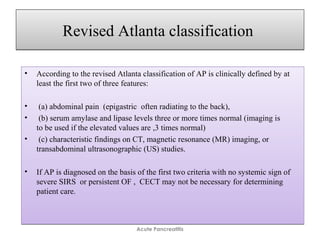
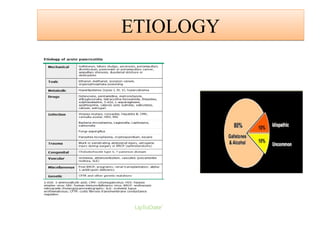
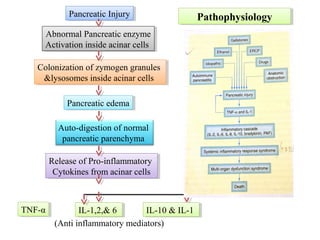
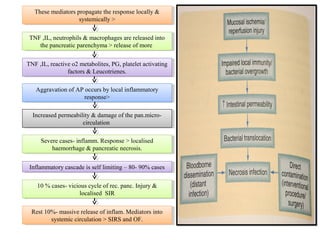
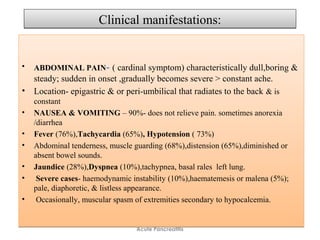
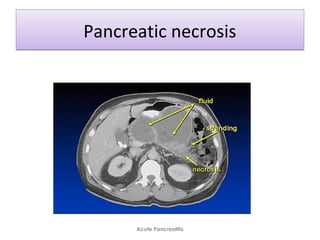
Acute pancreatitis is a potentially lethal condition that requires careful treatment and management. It involves sudden inflammation of the pancreas that can lead to the release of digestive enzymes within the abdomen. These enzymes can damage normal tissues, especially fat, and cause inflammation. The document discusses definitions of acute pancreatitis and classifications based on severity. Mild cases involve only inflammation while more severe cases can lead to pancreatic necrosis and organ failure. Treatment depends on the classification and complications. The pathogenesis involves trypsinogen activation within pancreas cells leading to autodigestion and an inflammatory response.


![ASSESSMENT OF SEVERITY –STAGING OF A.PASSESSMENT OF SEVERITY –STAGING OF A.P
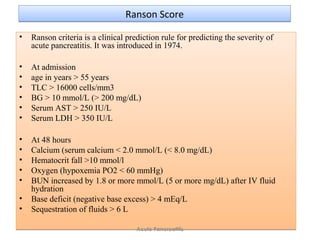
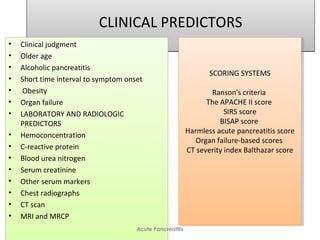
• Ranson Scoring
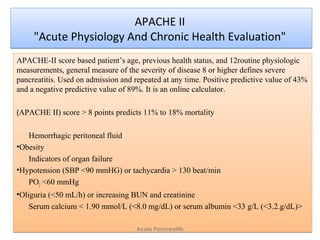
• Acute Physiology and Chronic Health Evaluation (APACHE) II,
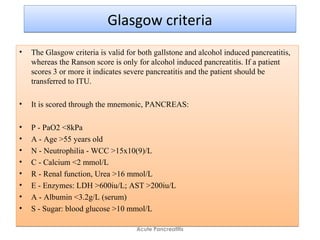
• Glasgow
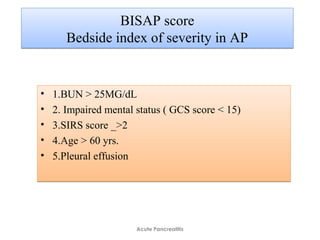
• BISAP Scoring
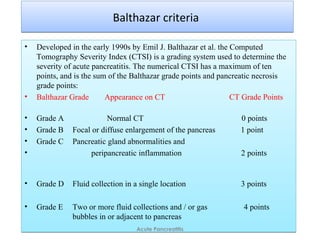
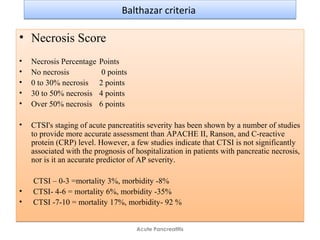
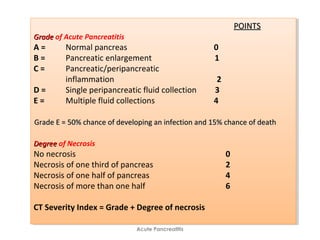
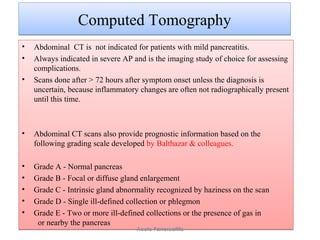
• Balthazar CTSI scoring systems.
• Each has advantages and disadvantages, and none is currently recognized as a
criterion standard.
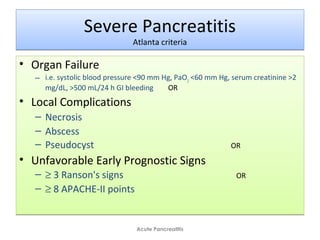
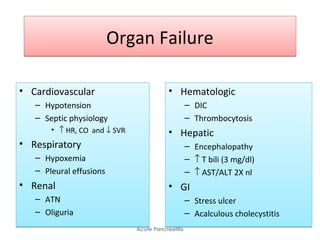
Evidence of ORGAN FAILURE:
Systolic B.P below 90 mm Hg,
Arterial partial pressure of oxygen [Pa O2] 60 mm Hg or lower,
Serum Creatinine level -2 mg/dL or lower,
GI bleeding amounting to 500 mL or more in 24 hrs
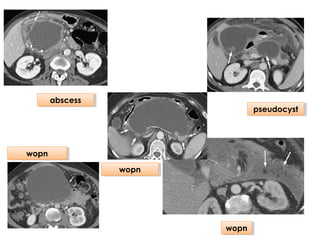
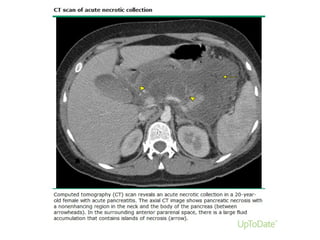
• Local complications (eg, necrosis, abscess, pseudocyst)
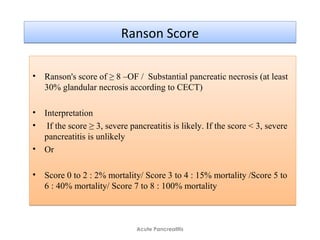
• Ranson score of 3 or higher or
• APACHE score of 8 or higher
•
• .
• Ranson Scoring
• Acute Physiology and Chronic Health Evaluation (APACHE) II,
• Glasgow
• BISAP Scoring
• Balthazar CTSI scoring systems.
• Each has advantages and disadvantages, and none is currently recognized as a
criterion standard.
Evidence of ORGAN FAILURE:
Systolic B.P below 90 mm Hg,
Arterial partial pressure of oxygen [Pa O2] 60 mm Hg or lower,
Serum Creatinine level -2 mg/dL or lower,
GI bleeding amounting to 500 mL or more in 24 hrs
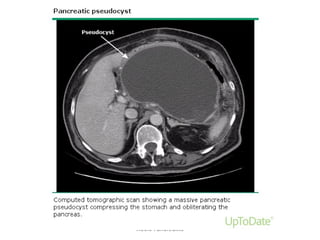
• Local complications (eg, necrosis, abscess, pseudocyst)
• Ranson score of 3 or higher or
• APACHE score of 8 or higher
•
• .
Acute Pancreatitis](https://image.slidesharecdn.com/acutepancreatitissp-160818072941/85/Acute-pancreatitis-SP-49-320.jpg)