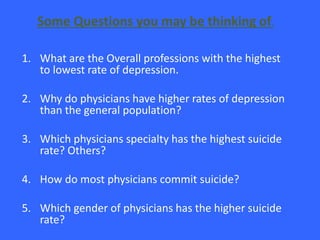
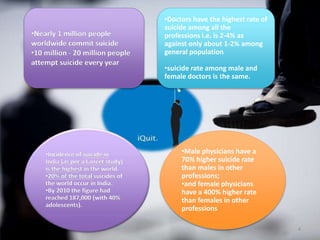
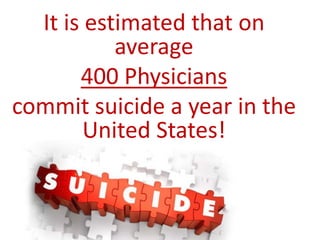
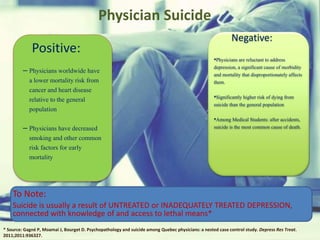
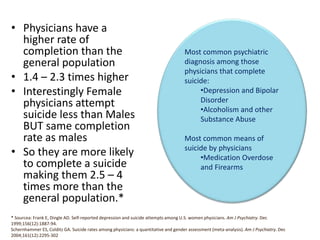
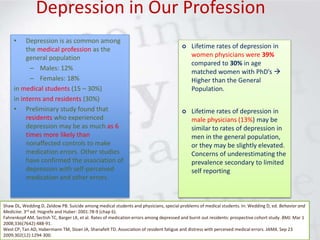
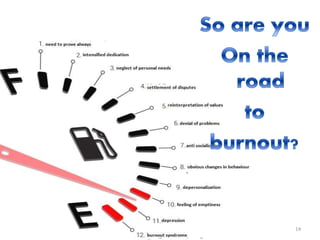
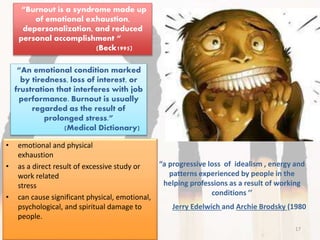
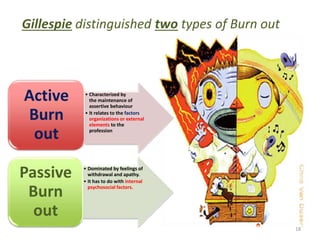
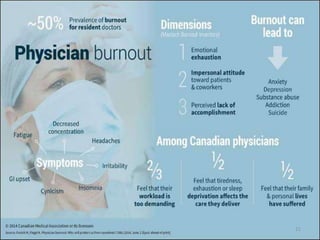
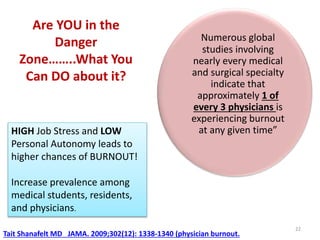
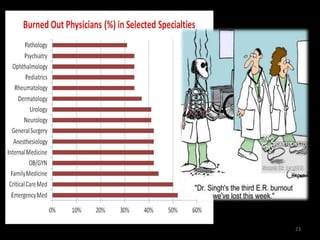
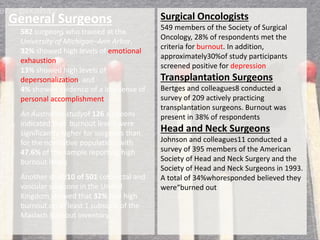
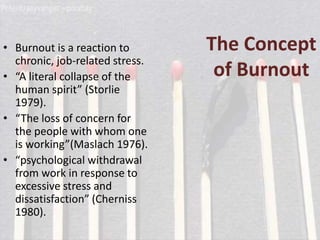
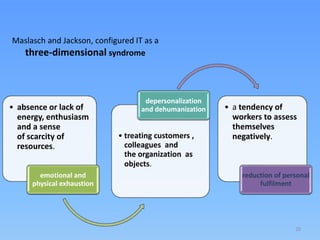
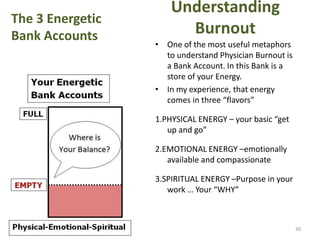
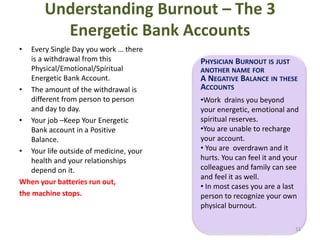
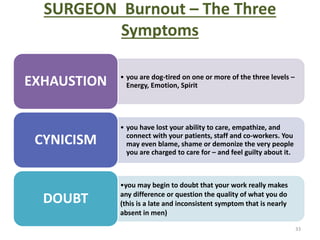
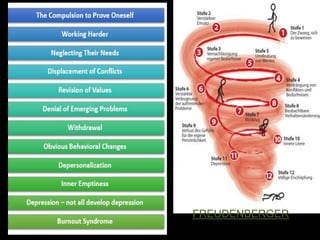
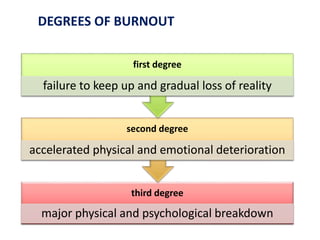
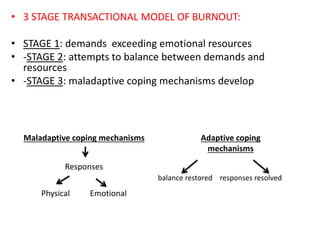
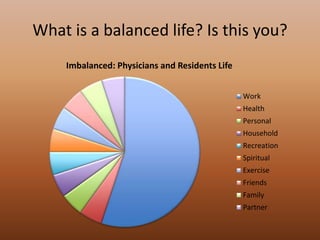
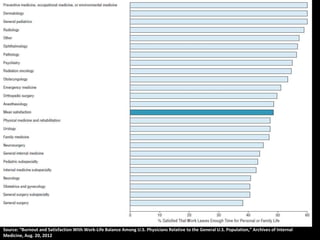
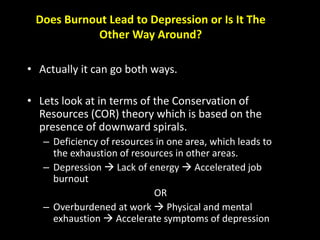
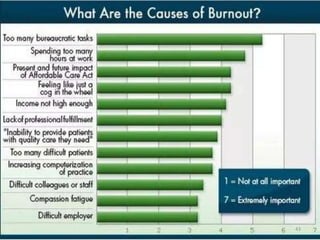
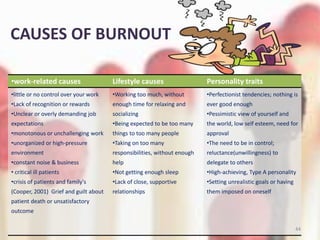
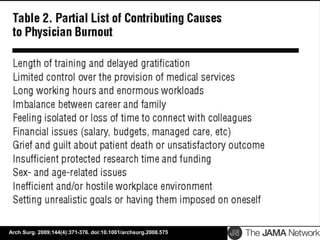
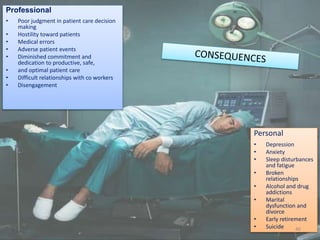
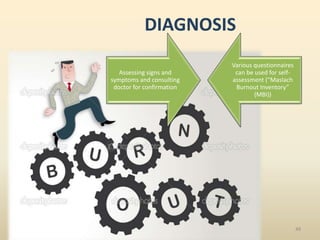
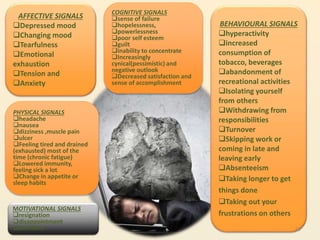
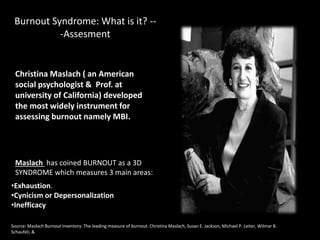
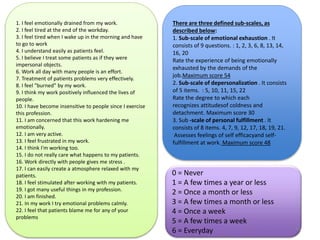
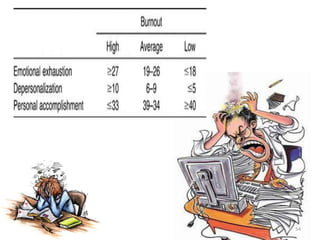
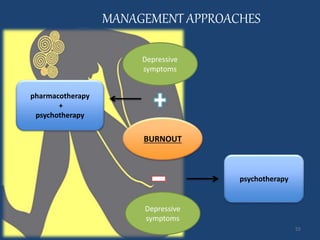
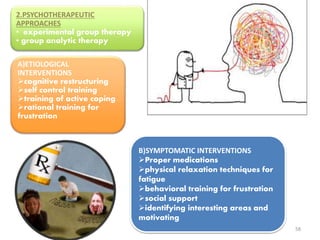
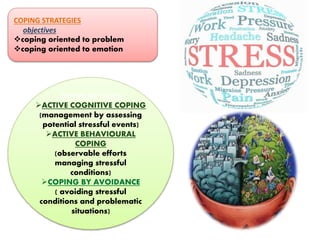
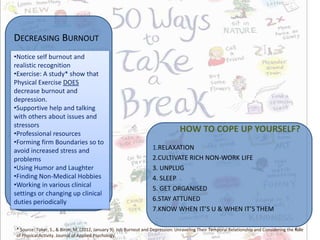
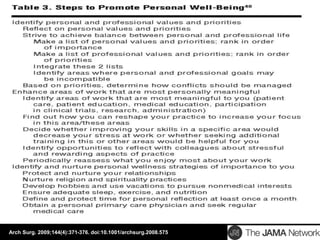
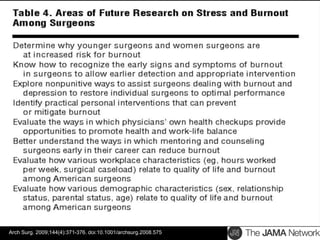
The document discusses the high rates of burnout and depression among physicians, particularly surgeons, highlighting the significant negative impacts on their mental health and professional performance. It notes that physicians have higher suicide rates compared to the general population, with specific disparities between genders and specialties. The document also addresses the causes of burnout, symptoms to watch for, and emphasizes the importance of addressing mental health issues within the medical profession.