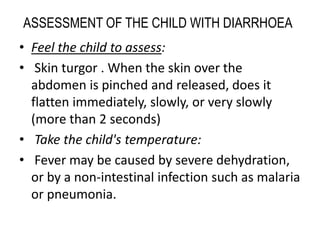
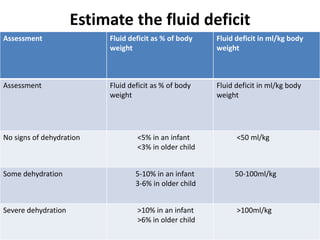
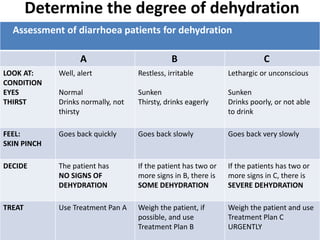
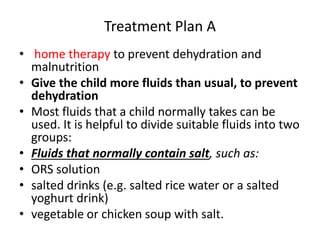
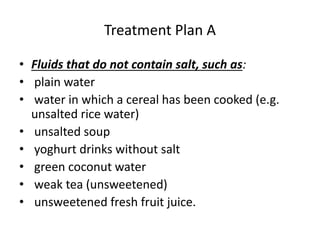
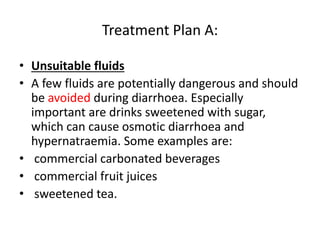
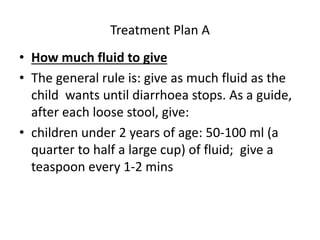
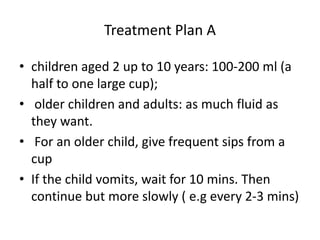
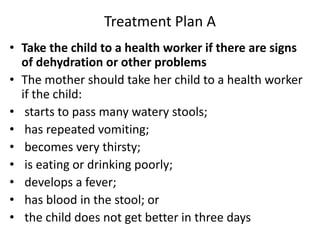
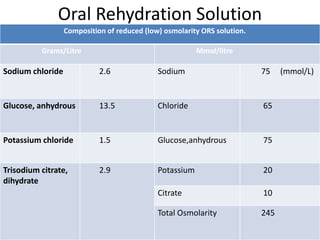
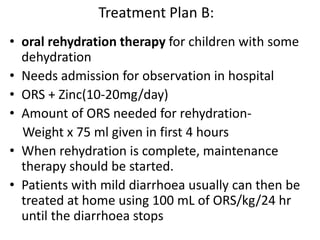
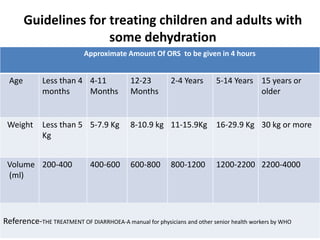
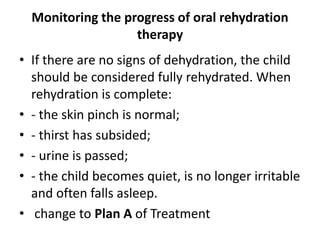
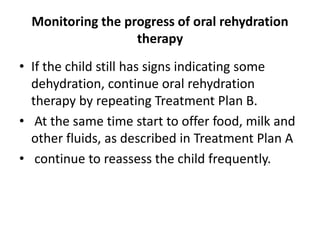
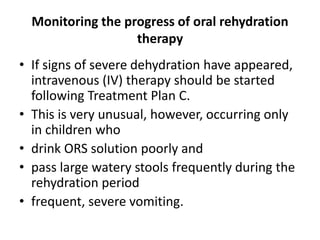
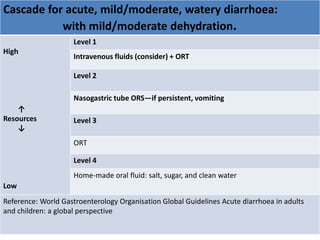
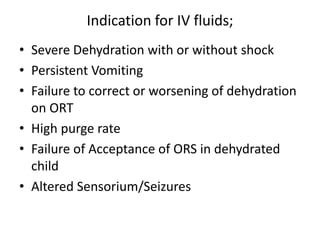
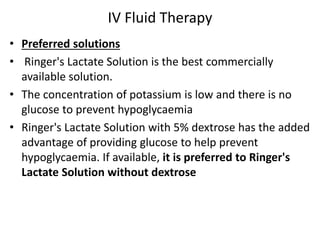
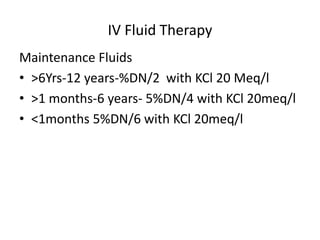
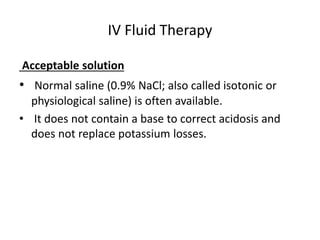
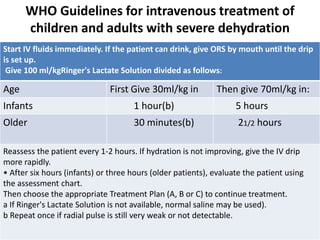
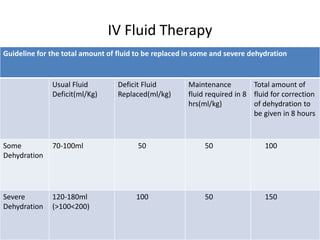
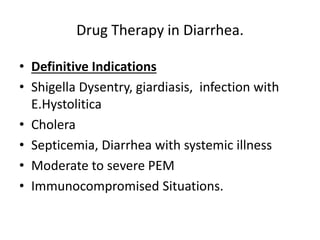
This document provides guidance on assessing and managing acute diarrhea in children. It describes how to take a thorough patient history and conduct a physical exam to evaluate dehydration. Three treatment plans are outlined for: no dehydration (plan A involving oral rehydration), some dehydration (plan B with oral and intravenous rehydration), and severe dehydration (plan C requiring intravenous therapy). The document provides details on oral rehydration solution composition and administration guidelines for rehydration based on a patient's age, weight, and degree of dehydration.