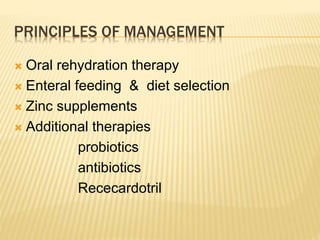
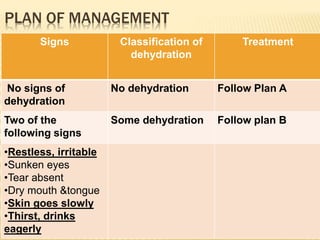
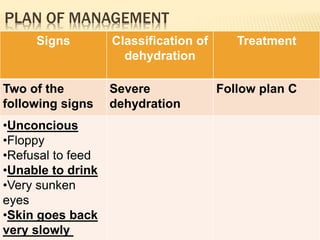
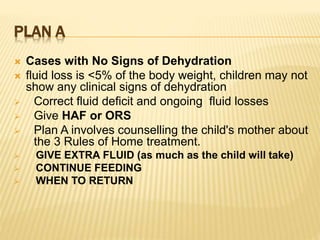
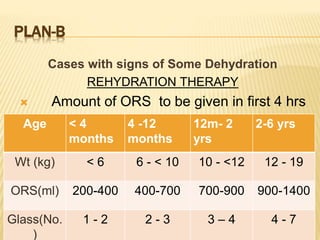
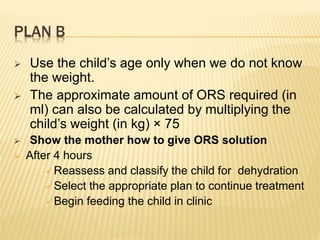
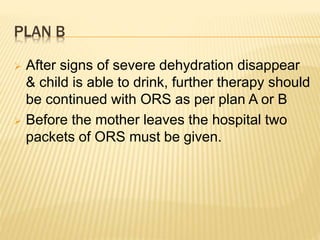
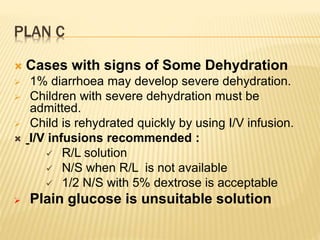
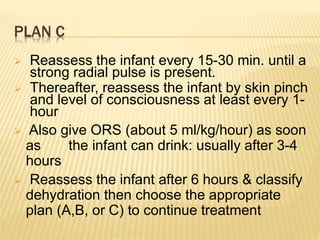
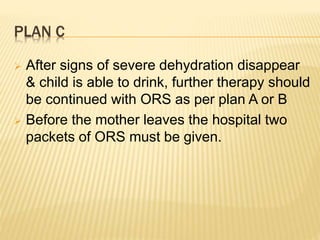
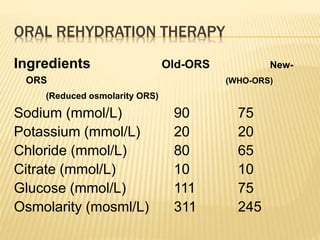
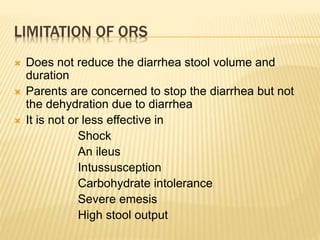
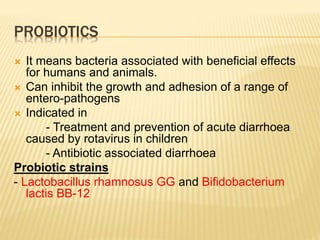
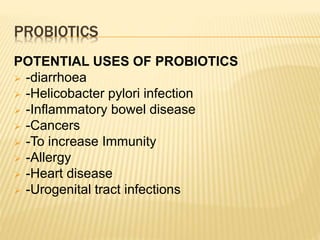
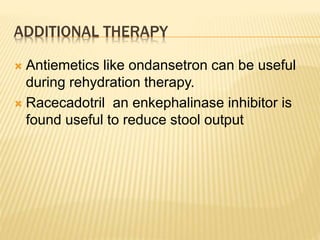
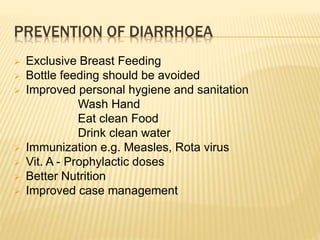
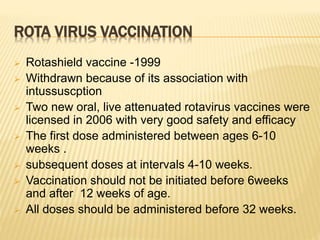
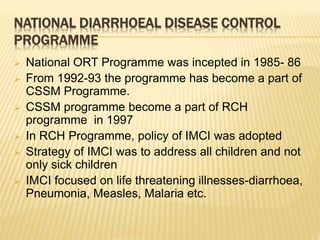
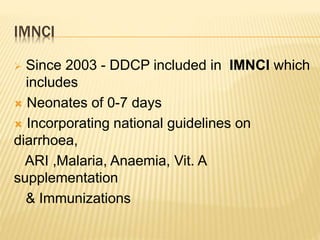
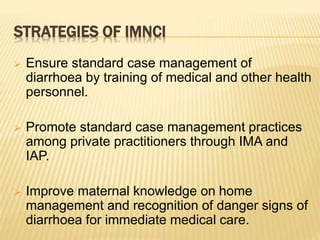
This document provides guidelines for the management of diarrhoea. It discusses oral rehydration therapy using oral rehydration solution and continued feeding. Zinc supplements are recommended. Additional therapies discussed include probiotics and antibiotics in certain cases. The document outlines plans for managing different levels of dehydration, from no dehydration to severe dehydration. It also discusses prevention strategies such as breastfeeding, handwashing, immunizations and vitamin A supplements.