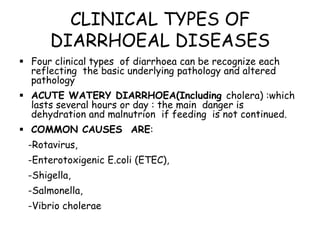
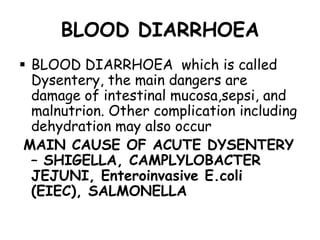
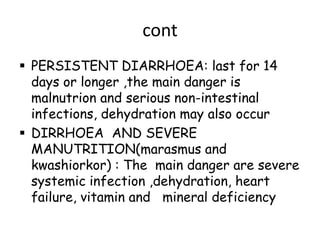
1. Diarrhea is caused by infections that imbalance the intestines' fluid and electrolyte processes, commonly from rotavirus in children. It can lead to dehydration, malnutrition, and death.
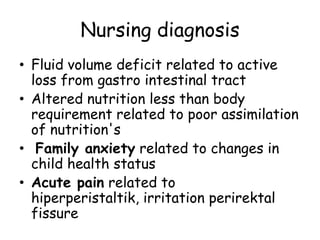
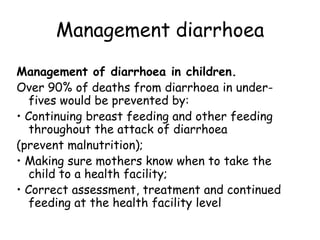
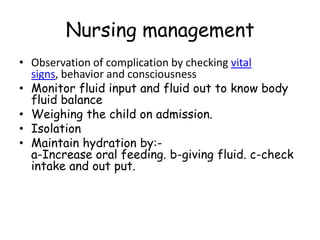
2. Nursing management of diarrhea involves monitoring for complications, maintaining hydration through oral rehydration and continued feeding, and treating any underlying infections.
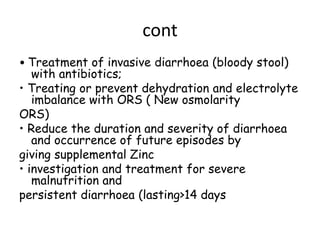
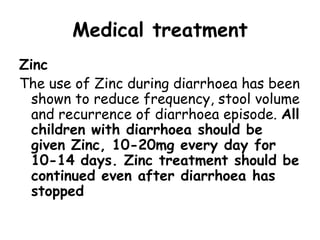
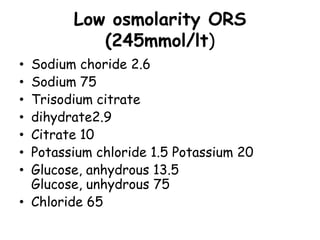
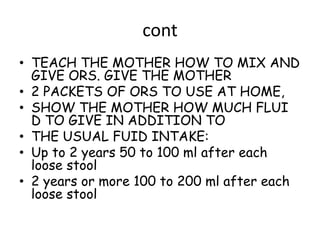
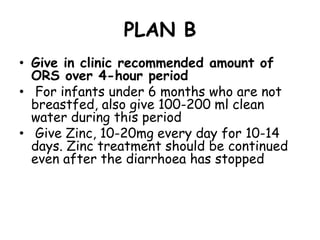
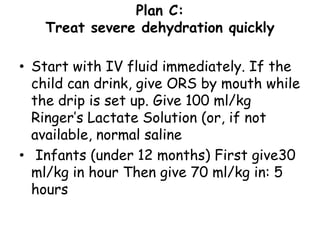
3. Treatment plans include oral rehydration with zinc at home, or intravenous rehydration in clinic for severe cases along with continued feeding and antibiotics if needed.