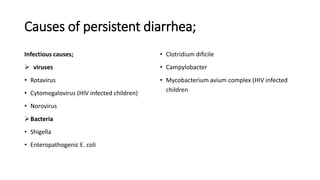
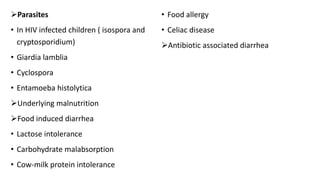
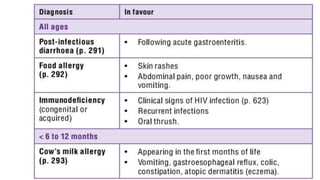
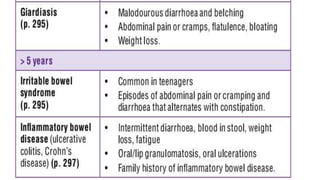
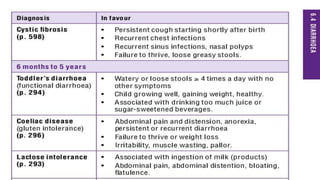
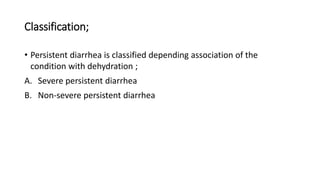
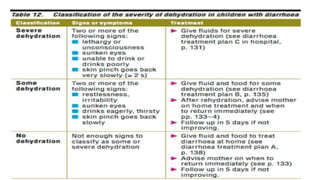
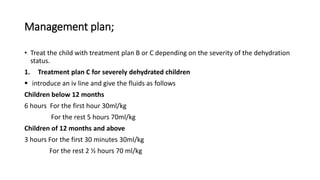
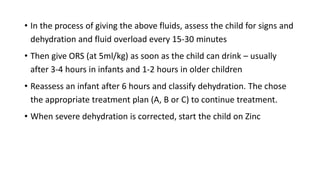
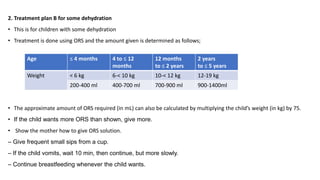
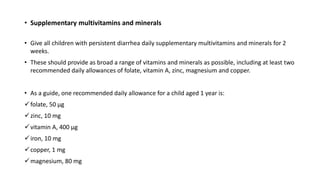
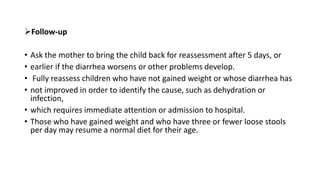
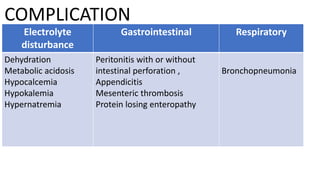
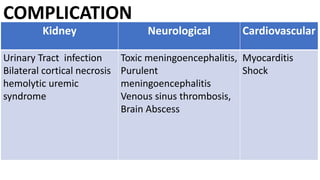
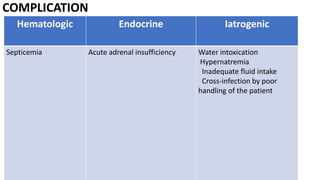
Persistent diarrhea is defined as diarrhea lasting 14 days or more. It can be caused by various infectious agents like viruses, bacteria, and parasites. It is classified as either severe persistent diarrhea, involving signs of dehydration requiring hospitalization, or non-severe persistent diarrhea treated as an outpatient. Management involves oral rehydration, continued feeding, zinc supplementation, and treating the underlying cause. Complications can involve various organ systems like the gastrointestinal, respiratory, neurological and hematological systems if not properly managed.