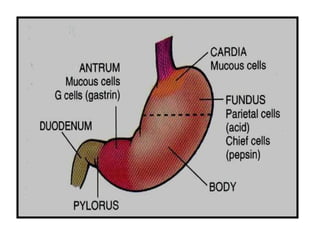
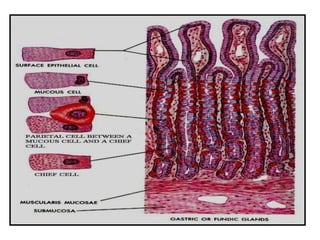
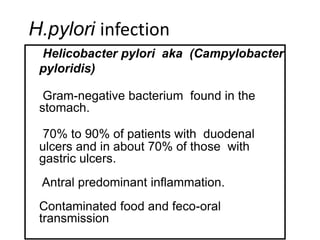
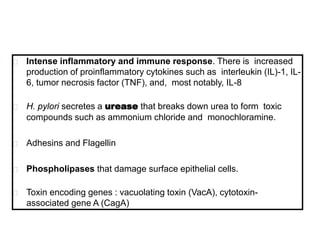
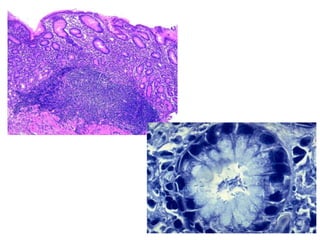
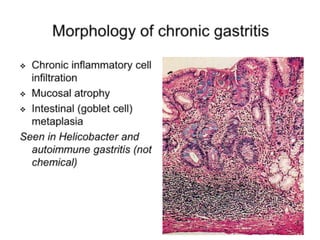
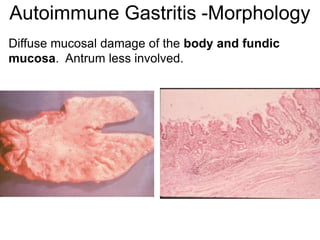
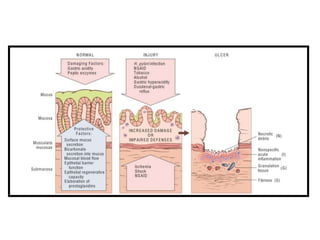
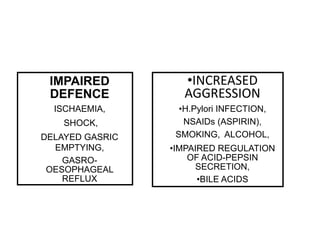
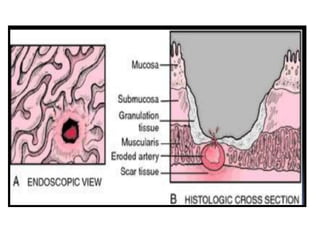
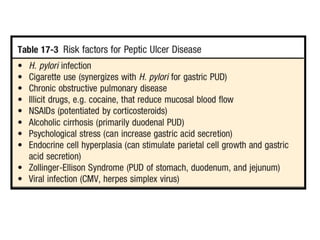
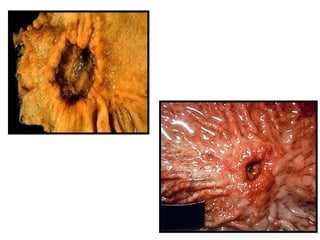
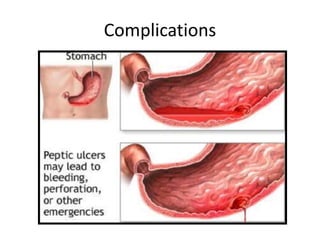
Chronic gastritis can be caused by H. pylori infection or autoimmune disorders. H. pylori infection leads to antral predominant gastritis and is associated with peptic ulcers. Untreated, it can progress to complications like MALToma or intestinal metaplasia, increasing cancer risk. Autoimmune gastritis affects the body and fundus, and may be associated with pernicious anemia or gastric carcinoid tumors due to loss of parietal cells. Both can result in atrophy, dysplasia, and intestinal metaplasia predisposing to gastric cancer. Peptic ulcers are chronic mucosal ulcers in the stomach or duodenum caused by an imbalance